Imagine struggling to breathe comfortably, especially when lying down. For many people with superior vena cava syndrome (SVCS), this experience is all too real. Orthopnea, or the difficulty of breathing while in a supine position, can be one of the most distressing symptoms associated with SVCS. This rare condition arises from compromised blood flow through the superior vena cava, leading to various troubling effects on the body.
Understanding how these two conditions intertwine is essential for both patients and caregivers alike. The journey begins with recognizing subtle signs that may escalate into more serious complications. From swollen limbs to severe orthopnea at night, awareness can empower timely intervention and treatment.
Join us as we explore orthopnea in superior vena cava syndrome—from its early symptoms to effective management strategies—creating a comprehensive guide for those affected by this challenging condition. Whether you’re seeking information for yourself or supporting a loved one, understanding SVCS could be key to enhancing quality of life and ensuring better health outcomes.
Understanding superior vena cava syndrome (SVCS): A rare cause of positional breathlessness
Superior vena cava syndrome (SVCS) occurs when there is obstruction or compression of the superior vena cava, a major vein responsible for returning blood from the upper body to the heart. This condition can lead to various symptoms, including facial swelling and upper extremity edema.
One of the most concerning manifestations is orthopnea, where individuals experience difficulty breathing while lying flat. The compromised blood flow affects oxygen saturation in the body and leads to discomfort during sleep or rest.
SVCS may arise from different causes, such as tumors, thrombosis, or infections that exert pressure on the superior vena cava. Lung cancer is one of the leading culprits but other malignancies and even benign conditions can contribute to this syndrome.
Understanding SVCS requires awareness of its underlying mechanisms and how they impact respiratory function. Recognizing these symptoms early on can guide patients toward appropriate medical evaluation and treatment options.
From subtle swelling to severe orthopnea: The progression of SVCS symptoms
Superior vena cava syndrome (SVCS) often begins subtly, with mild symptoms that can easily be overlooked. Patients may notice slight swelling in the face, neck, or upper extremities. This initial sign is due to increased pressure in the superior vena cava, which impedes normal blood flow.
As SVCS progresses, individuals might experience more pronounced swelling and discomfort. The skin may appear tight and shiny. Alongside physical changes, some people report feelings of heaviness in their arms or a sense of fullness around their necks. These signs are crucial indicators that warrant closer attention.
Orthopnea develops as fluid accumulates and pressure builds further within the chest cavity. Patients often find it increasingly challenging to breathe comfortably while lying flat. Sleep disturbances become common as they seek alternative positions for relief.
In advanced cases of SVCS, orthopnea can escalate into severe breathing difficulties during even minor exertion. Understanding this progression aids timely recognition and intervention for those affected by this complex condition.
Diagnostic journey: Identifying SVCS as the cause of orthopnea
Identifying superior vena cava syndrome (SVCS) as the cause of orthopnea involves a careful diagnostic journey. Patients often present with symptoms like difficulty breathing while lying down, which can be mistaken for other respiratory issues. A thorough medical history and physical examination are essential first steps.
Doctors may note signs such as facial swelling or distended neck veins during their assessment. These observations raise suspicion for SVCS, prompting further investigation. Imaging tests play a crucial role in this process; chest X-rays and CT scans can reveal obstructions or abnormalities in the superior vena cava.
Additionally, blood tests help rule out other conditions that could mimic SVCS symptoms. Oncological evaluations may also be indicated since cancers are a common underlying cause of this syndrome.
Once doctors piece together these findings, they can establish an accurate diagnosis of SVCS linked to orthopnea. Early detection is vital to manage symptoms effectively and prevent complications associated with this serious condition.
Treatment approaches: Addressing the underlying cause to improve breathing
Treatment for orthopnea in Superior Vena Cava Syndrome often focuses on addressing the underlying cause of the obstruction. This might involve managing tumors compressing the superior vena cava or treating blood clots that obstruct blood flow. In some cases, medical interventions like chemotherapy can help shrink malignancies, easing pressure on surrounding structures.
For patients with significant clotting issues, anticoagulant therapy may be initiated to dissolve existing clots and prevent new ones from forming. Additionally, stenting procedures are available to relieve compression by placing a small tube within the vein, allowing for improved blood flow.
Symptom management is equally important. Diuretics can reduce fluid build-up and swelling associated with SVCS, helping improve overall comfort during daily activities. Furthermore, corticosteroids might be prescribed to decrease inflammation around the affected area.
Lifestyle modifications also play a crucial role in treatment plans. Elevating the upper body during sleep and avoiding tight clothing can significantly alleviate symptoms of orthopnea while enhancing quality of life for those living with SVCS.
Managing orthopnea: Strategies for comfortable sleep and daily activities
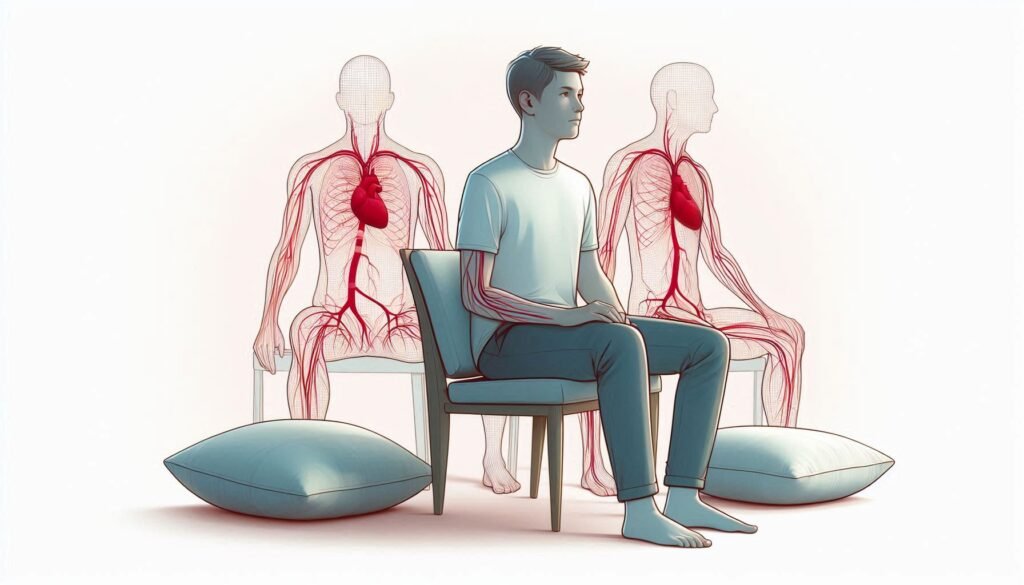
Managing orthopnea in Superior Vena Cava Syndrome requires thoughtful strategies to ensure comfortable sleep and daily activities. Elevating the head during sleep can significantly alleviate symptoms. Using a wedge pillow or adjustable bed helps promote easier breathing by reducing pressure on the chest and facilitating better blood flow.
Creating an organized environment also aids in managing orthopnea. Keeping essential items within reach minimizes unnecessary movements that could trigger breathlessness. Consider using assistive devices, such as grab bars or mobility aids, to enhance safety while moving around the home.
Daytime routines should incorporate regular breaks to prevent fatigue and shortness of breath. Engaging in gentle exercises like walking or stretching can improve circulation without overwhelming the body. However, it’s vital to listen to one’s limits and adjust activity levels according to individual comfort.
Incorporating relaxation techniques into daily life is beneficial as well. Practices such as deep breathing exercises, meditation, or yoga can reduce stress and promote overall lung function, making it easier for those affected by orthopnea in SVCS to navigate their day-to-day lives with greater ease.
Complications of untreated SVCS: Beyond breathing difficulties
Untreated superior vena cava syndrome (SVCS) can lead to a range of serious complications beyond breathing difficulties. One significant concern is the risk of swelling in the upper body and face, known as edema. This swelling can become uncomfortable and may hinder daily activities.
As pressure increases within the veins, patients might experience headaches or dizziness due to disrupted blood flow to the brain. These symptoms often arise from increased intracranial pressure, which can be alarming for those affected.
In more severe cases, untreated SVCS can result in venous thrombosis, where blood clots form due to stagnant blood flow. This condition poses additional risks such as pulmonary embolism if a clot dislodges and travels to the lungs.
Moreover, chronic oxygen deprivation from impaired circulation may lead to cardiac strain over time. The heart works harder than usual to compensate for reduced blood return, potentially resulting in heart failure if left unaddressed. Recognizing these complications early is crucial for effective management and treatment strategies.
Emergency situations: When SVCS-related orthopnea becomes life-threatening
Orthopnea in Superior Vena Cava Syndrome can escalate into a life-threatening emergency. Patients may experience sudden worsening of breathlessness when lying flat, leading to significant respiratory distress. This compromised blood flow affects not only breathing but also vital organ function.
Signs that indicate an urgent situation include rapid heart rate, confusion, and cyanosis—where lips or fingers turn blue due to lack of oxygen. These symptoms suggest that the body is struggling to compensate for reduced circulation in the upper body. Immediate medical attention is crucial at this point.
Additionally, if swelling around the neck or face suddenly increases, it may signal severe obstruction requiring prompt intervention. Such changes could mean imminent risk for airway compromise as pressure builds on surrounding structures.
Timely diagnosis and treatment are essential in these emergencies to prevent further complications like stroke or cardiac arrest. Recognizing these warning signs can save lives and lead to better management strategies for those affected by SVCS-related orthopnea.
Long-term outlook: Can orthopnea be completely resolved in SVCS?
The long-term outlook for orthopnea in Superior Vena Cava Syndrome (SVCS) varies significantly among individuals. Some patients experience substantial relief after appropriate treatment, while others may face ongoing challenges. The key factor is the underlying cause of SVCS, which often includes malignancies or other vascular conditions.
When addressed early and effectively, many patients see improvement in their symptoms. Treatments such as stenting or chemotherapy can alleviate pressure on the superior vena cava, leading to better blood flow and reduced orthopnea. However, complete resolution isn’t guaranteed for everyone.
In cases where SVCS is due to chronic conditions like tumors that are difficult to manage, persistent issues might remain. Lifestyle modifications and supportive therapies can help mitigate symptoms but may not fully eliminate them.
Regular follow-ups with healthcare providers are crucial for monitoring progress. Tailored care plans can enhance quality of life even when complete resolution isn’t achievable. Understanding individual circumstances plays a significant role in managing expectations around orthopnea related to SVCS.
Supportive care: Improving quality of life for SVCS patients
Supportive care plays a crucial role in enhancing the quality of life for patients with superior vena cava syndrome (SVCS). This approach focuses on alleviating symptoms and providing comfort rather than solely treating the underlying cause. By addressing the challenges posed by orthopnea, healthcare providers can help patients regain a sense of normalcy.
Breathing exercises tailored to each patient’s needs can significantly improve lung capacity and reduce feelings of breathlessness. Techniques such as pursed-lip breathing or diaphragmatic breathing may offer relief during daily activities. Additionally, maintaining an optimal sleeping position—such as propping up with pillows—can alleviate nighttime discomfort associated with orthopnea.
Another essential aspect is emotional support. Many SVCS patients experience anxiety related to their condition, making it vital for caregivers and family members to provide reassurance and understanding. Support groups also serve as valuable resources where individuals can share experiences and coping strategies.
Nutritional counseling is equally important, emphasizing balanced meals that promote overall health. A well-rounded diet contributes not just to physical strength but also positively impacts mental well-being amid challenging circumstances.
Research update: New directions in understanding and treating SVCS
Current research is expanding our understanding of orthopnea in superior vena cava syndrome (SVCS) and its treatment options. Scientists are investigating advanced imaging techniques that can better visualize blood flow dynamics in affected patients. These innovations may lead to earlier diagnosis and more effective interventions.
Clinical trials are also exploring new medications aimed at alleviating symptoms associated with SVCS, including targeted therapies for the underlying conditions such as cancer or heart disease that often contribute to the syndrome. Moreover, researchers are examining the role of minimally invasive procedures like stenting to relieve pressure on the superior vena cava itself.
As knowledge about SVCS grows, so too does hope for improved outcomes. Enhanced awareness among healthcare providers can facilitate quicker identification and management of this condition, ultimately leading to a better quality of life for those suffering from orthopnea due to SVCS. Continued investment in research will ensure that future strategies not only address breathing difficulties but also tackle root causes effectively, paving the way for comprehensive care solutions moving forward.


