Imagine drifting off to sleep, only to find that your breathing halts repeatedly throughout the night. This scenario is all too real for millions dealing with Obstructive Sleep Apnea (OSA). It’s more than just a nuisance; it can impact your health and quality of life in significant ways. Understanding OSA is crucial not only for those who suffer from it but also for their loved ones.
In this article, we will explore what obstructive sleep apnea is, its symptoms, risk factors, and the various treatment options available. Whether you suspect you might have OSA or want to support someone who does, you’re in the right place! Let’s delve into the world of sleep apnea and uncover how it affects lives around us every day.
What is Obstructive Sleep Apnea? A Simple Explanation
Obstructive Sleep Apnea (OSA) is a common sleep disorder characterized by repeated interruptions in breathing during sleep. These pauses occur when the muscles at the back of your throat relax excessively, leading to a temporary blockage of the airway.
“What Are the Hidden Dangers of Sleep Apnea? Expert Guide”
When airflow is obstructed, oxygen levels drop, triggering the brain to wake you up just enough to reopen your airway. This cycle can happen multiple times throughout the night, often without you even realizing it.
As a result, individuals with OSA experience fragmented sleep. They may struggle with daytime fatigue and reduced concentration due to not achieving restorative rest. Recognizing OSA early on is vital for effective management and prevention of related health issues.
The Silent Struggle: Common Symptoms of Sleep Apnea
Obstructive Sleep Apnea (OSA) often creeps in unnoticed, masking its presence with subtle signs. Many individuals may not realize they are affected until their partner points out the snoring or gasping for breath during sleep.
“Why Does Atelectasis Cause Breathing Problems? Understanding Lung Collapse”
Frequent daytime fatigue is a hallmark symptom. You might feel like you haven’t slept at all, even after a full night in bed. This exhaustion can hinder daily activities and reduce productivity.
Morning headaches are also common among those suffering from OSA. These headaches result from interrupted sleep cycles and decreased oxygen flow to the brain.
Mood swings and irritability can arise too. The constant struggle for restful sleep takes its toll on emotional well-being.
Night sweats may occur as well, leaving you feeling uncomfortable throughout the night. Recognizing these symptoms early is crucial for seeking appropriate treatment and improving your overall health.
Snoring and Beyond: Key Signs You Might Have OSA
Snoring is often the first sign of Obstructive Sleep Apnea (OSA). While many people snore occasionally, those with OSA experience loud and disruptive snoring that can wake them or their partners.
“What Makes Pulmonary Fibrosis Progressive? Treatment & Management”
However, it doesn’t stop there. Individuals may also notice sudden pauses in breathing during sleep. These interruptions are often followed by choking or gasping for air.
Excessive daytime drowsiness is another red flag. If you find yourself struggling to stay awake during daily activities, it could be a sign of disrupted nighttime rest.
Mood changes can also occur due to poor quality sleep. Irritability and difficulty concentrating may point toward underlying issues like OSA.
“How Does Myasthenia Gravis Affect Your Breathing? Key Information”
If you’re experiencing any combination of these symptoms, it’s essential to consult a healthcare professional for evaluation and potential diagnosis of obstructive sleep apnea.
Risk Factors: Who’s Most Likely to Develop Sleep Apnea?
Certain individuals are more susceptible to developing obstructive sleep apnea (OSA). Understanding these risk factors can be crucial for early intervention.
“What Causes Sudden Dyspnea? Understanding Breathing Difficulties”
Age is a significant contributor; OSA often becomes more prevalent in middle-aged adults. Hormonal changes and muscle tone loss play roles as we age.
Gender also matters. Men are generally more likely to experience sleep apnea than women, though the risk increases for women after menopause.
Obesity stands out as one of the leading indicators. Excess weight contributes to fatty deposits around the neck, which can obstruct airflow during sleep.
Family history should not be overlooked either. Genetics may influence an individual’s likelihood of developing OSA.
“Why Is My Breathing So Fast? Understanding Tachypnea”
Additionally, certain medical conditions such as hypertension and diabetes elevate risks. Lifestyle choices like smoking and alcohol consumption further increase vulnerability to this condition.
The Weight Connection: Obesity and Sleep Apnea
Obesity plays a significant role in the development of obstructive sleep apnea (OSA). Excess body weight can lead to fatty deposits around the neck and throat, which may narrow airways during sleep. This narrowing increases resistance to airflow, prompting episodes where breathing stops.
Research indicates that individuals with obesity are at a higher risk of experiencing OSA. The severity often correlates directly with BMI (Body Mass Index); as weight increases, so does the likelihood of airway obstruction.
“What Are the Dangers of Hypoxemia? Signs You Need Medical Help”
Moreover, losing even a small amount of weight can improve symptoms or reduce the severity of OSA. Weight loss helps decrease pressure on the upper airway, aiding in easier breathing at night.
Addressing obesity through diet and exercise not only promotes overall health but also significantly enhances sleep quality for those affected by this condition. Understanding this connection is crucial in managing both obesity and obstructive sleep apnea effectively.
Anatomy Matters: Physical Traits That Increase OSA Risk
Anatomy plays a significant role in the development of Obstructive Sleep Apnea (OSA). Certain physical traits can increase an individual’s risk, making it essential to understand these factors.
One primary trait is a thick neck circumference. Individuals with larger necks may experience more airway obstruction during sleep. This extra tissue can compress the throat and block airflow.
“How Do Chest Wall Disorders Impact Breathing? Complete Guide”
Facial structure also matters. A recessed chin or overbite can lead to tighter airways. Additionally, enlarged tonsils and adenoids are common culprits in both adults and children.
Body fat distribution influences OSA risk as well. Fat accumulation around the neck area puts pressure on the airway during sleep, worsening symptoms.
Age contributes to OSA prevalence; muscle tone decreases naturally over time, leading to increased susceptibility for many individuals as they grow older. Understanding these anatomical factors is crucial for early detection and effective management of OSA.
Diagnosing the Problem: Sleep Studies and OSA
Diagnosing Obstructive Sleep Apnea (OSA) often begins with a comprehensive sleep study. This assessment is crucial for understanding how your body behaves during sleep.
There are two primary types of sleep studies: in-lab polysomnography and home sleep tests. In-lab studies involve spending the night at a specialized facility, where healthcare professionals monitor various parameters such as brain waves, heart rate, and oxygen levels.
“What Causes Altitude Sickness? Prevention & Treatment Guide”
Home sleep tests offer more convenience. They allow patients to undergo monitoring in their own beds using portable devices that track breathing patterns and other vital signs. Both methods provide valuable insights into whether OSA is present.
After collecting data, doctors analyze the results to determine the severity of apnea episodes and recommend appropriate treatment options based on individual needs. Early diagnosis can significantly improve quality of life for those affected by this condition.
Home Sleep Tests: A Convenient Option for OSA Diagnosis
Home sleep tests have emerged as a practical solution for diagnosing obstructive sleep apnea (OSA) in the comfort of your own home. These tests are designed to monitor key factors such as breathing patterns, oxygen levels, and heart rate while you sleep.
Unlike traditional sleep studies that require an overnight stay in a lab, home tests are user-friendly and typically involve simple devices. You may wear a small recording device or use sensors placed on your body before going to bed.
The convenience of this approach allows individuals to undergo testing without disrupting their normal routines. Results can often be reviewed quickly by healthcare professionals, leading to timely diagnosis and treatment options.
While not all cases of OSA can be accurately assessed through home testing, it serves as an effective first step for many individuals seeking answers about their nighttime struggles with breathing.
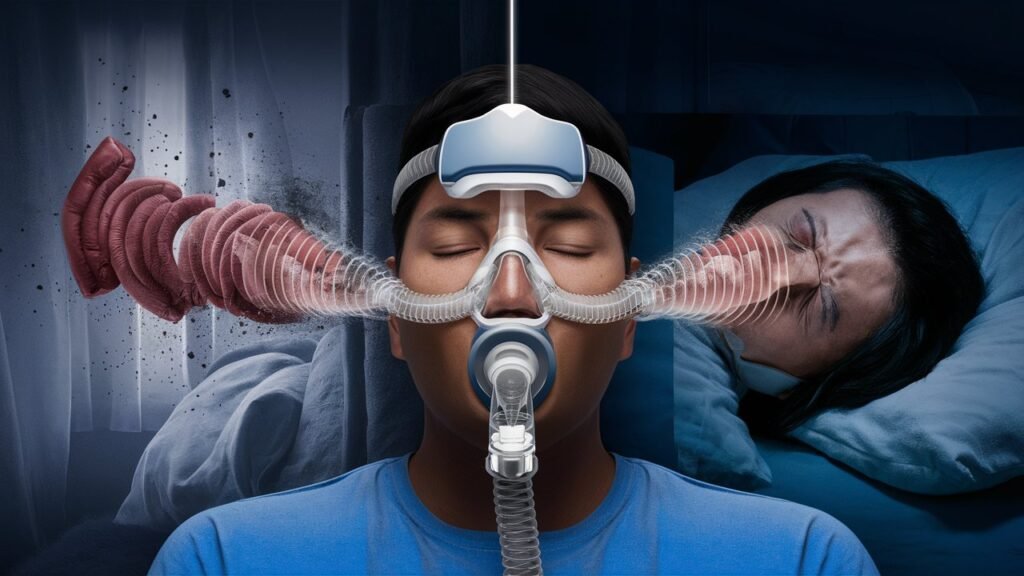
CPAP Therapy: The Gold Standard for Treating Sleep Apnea
CPAP therapy, or Continuous Positive Airway Pressure, has emerged as the gold standard for managing obstructive sleep apnea (OSA). This treatment involves wearing a mask connected to a machine that delivers a steady stream of air. The airflow keeps the airway open during sleep, preventing pauses in breathing.
Many patients find CPAP effective and often experience immediate improvements in their quality of sleep. With consistent use, symptoms like snoring and daytime drowsiness can significantly diminish.
The devices come with various features such as adjustable pressure settings and built-in humidifiers. These advancements enhance comfort for users who may struggle with traditional masks.
Regular follow-ups with healthcare providers ensure optimal settings adjusted to individual needs. While some might face an adjustment period when starting CPAP therapy, many report feeling more alert and energized once they adapt to this life-changing treatment option.
Beyond CPAP: Other Treatment Options for OSA
While CPAP therapy is the gold standard for treating Obstructive Sleep Apnea (OSA), it’s not the only option. For those who find CPAP uncomfortable or ineffective, several alternatives exist.
Oral appliances are a popular choice. These custom-fit devices reposition the jaw and tongue to keep airways open during sleep. Many patients find them more comfortable than CPAP machines.
Positional therapy can also be effective. This involves encouraging side-sleeping rather than back-sleeping, which often exacerbates OSA symptoms.
For some, weight loss may lead to significant improvements. Shedding excess pounds can reduce fatty deposits around the neck and throat, easing airway obstruction.
Certain medications may help alleviate mild cases of OSA by reducing muscle relaxation in the throat during sleep. Always consult with a healthcare provider to explore these options tailored to individual needs and circumstances.
Lifestyle Changes: Natural Ways to Improve Sleep Apnea
Making lifestyle changes can significantly improve symptoms of Obstructive Sleep Apnea (OSA). One effective strategy is to maintain a healthy weight. Shedding excess pounds often leads to reduced pressure on the airway, enhancing breathing during sleep.
Regular exercise plays a vital role too. Engaging in physical activities not only aids weight management but also improves overall sleep quality. Aim for at least 30 minutes most days.
Dietary habits are equally important. A balanced diet rich in fruits, vegetables, and whole grains can promote better sleeping patterns. Avoiding heavy meals and alcohol close to bedtime helps prevent disruptions.
Sleep position matters as well. Sleeping on your side rather than your back can reduce airway obstruction significantly.
Implementing consistent sleep schedules fosters better restfulness too. Going to bed and waking up at the same time each day trains the body for optimal performance during nighttime hours.
The Surgery Question: When to Consider Surgical Options for OSA
Surgery for obstructive sleep apnea (OSA) isn’t the first line of defense but may be necessary in some cases. When other treatments, like CPAP therapy or lifestyle changes, fail to provide relief, surgical options can come into play.
Candidates for surgery often exhibit anatomical abnormalities that contribute to their condition. This includes enlarged tonsils or adenoids and structural issues within the jaw. If these traits are identified, a surgical evaluation becomes essential.
The most common procedures include uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the throat, and maxillomandibular advancement (MMA), which repositions the jaw to improve airway size.
Before considering surgery, it’s crucial to weigh potential benefits against risks carefully. Consulting with a specialist can help determine if this path is suitable based on individual circumstances and health status.
Sleep Apnea in Children: A Different Beast
Sleep apnea in children is often overlooked. However, it can significantly impact their health and development. Unlike adults, kids may not exhibit classic symptoms like loud snoring. Instead, they might show signs of restless sleep or frequent awakenings.
Parents should look for behavioral changes too. Increased irritability, difficulty concentrating at school, and excessive daytime sleepiness could all indicate a problem with breathing during the night.
Enlarged tonsils or adenoids are common culprits behind pediatric obstructive sleep apnea (OSA). These conditions can block airflow and disrupt normal breathing patterns.
Diagnosis usually involves a thorough evaluation by a pediatrician or a specialist. Sleep studies tailored for children help pinpoint the severity of OSA in younger patients.
Treatments vary based on age and severity but often include lifestyle adjustments or surgical options to remove obstructions. Early intervention can lead to better outcomes for children’s overall well-being.
Untreated OSA: The Serious Health Risks You Can’t Ignore
Untreated obstructive sleep apnea (OSA) poses serious health risks that can impact your overall well-being. One of the most concerning consequences is cardiovascular disease. Repeated interruptions in breathing elevate blood pressure and strain the heart, increasing the risk of heart attacks and strokes.
Metabolism also suffers in those with untreated OSA. The condition disrupts hormone levels, leading to insulin resistance and a higher likelihood of type 2 diabetes. This metabolic imbalance can contribute to weight gain, further aggravating sleep apnea.
Mental health issues are another significant concern. Chronic fatigue from poor sleep quality often leads to depression and anxiety, affecting daily life.
Cognitive function may degrade over time due to lack of restorative sleep. Memory problems and difficulty concentrating become common complaints among individuals suffering from untreated OSA. It’s crucial not to overlook these potential dangers associated with this silent epidemic.
Heart Health and OSA: Understanding the Connection
Obstructive Sleep Apnea (OSA) significantly impacts heart health. During sleep, breathing interruptions lead to decreased oxygen levels. This can strain the cardiovascular system.
The body responds to these drops in oxygen by raising blood pressure and increasing heart rate. Over time, this chronic stress contributes to hypertension and can lead to serious conditions like heart disease or stroke.
Additionally, OSA is linked with irregular heartbeats known as arrhythmias. These disruptions can further complicate existing heart issues.
People with untreated OSA often experience increased inflammation throughout their bodies, which also affects the cardiovascular system negatively.
Recognizing symptoms of sleep apnea is crucial for early intervention. Treatment not only improves sleep quality but also promotes overall heart health, making awareness vital for those at risk.
Daytime Drowsiness: The Hidden Danger of Sleep Apnea
Daytime drowsiness is one of the most insidious effects of obstructive sleep apnea (OSA). Many people don’t realize that frequent fatigue isn’t just a side effect of poor sleep but can be a serious symptom of this condition.
When breathing stops during sleep, oxygen levels drop. This leads to fragmented rest and disrupted REM cycles. As a result, individuals often wake up feeling unrefreshed.
Chronic daytime drowsiness impacts daily life significantly. It can hinder productivity at work or school and increase the risk of accidents while driving or operating machinery. The brain struggles to function optimally without sufficient restorative sleep.
Moreover, the emotional toll should not be overlooked. Increased irritability and mood swings are common among those who battle excessive daytime sleepiness due to OSA. Recognizing these challenges is essential for finding effective management strategies and seeking help.
Partners and Sleep Apnea: When Your Loved One Has OSA
Living with a partner who has obstructive sleep apnea (OSA) can be challenging. The condition not only affects the person experiencing it but also impacts their loved ones. Understanding OSA is key to offering support.
Communication is vital. Talk openly about how OSA influences nightly routines and overall health. Encourage your partner to seek medical advice if they haven’t already done so.
Sleep disruptions are common, which might lead to frustrations or misunderstandings at night. Consider creating separate sleeping arrangements temporarily if snoring or breathing interruptions are severe.
Educating yourself on treatment options can help you assist in their journey toward better sleep quality. Whether it’s using CPAP therapy or lifestyle changes, being involved shows your commitment.
Prioritize self-care for yourself as well. Supporting someone with a chronic condition can be taxing; ensure you’re taking time for your own well-being too.
Sleep Apnea and Mental Health: The Surprising Link
Obstructive Sleep Apnea (OSA) doesn’t just affect your sleep; it can also take a toll on mental health. Research indicates that people with OSA are at higher risk for anxiety and depression.
The disrupted sleep patterns caused by OSA lead to fatigue, irritability, and cognitive difficulties. This constant struggle can create a vicious cycle where poor mental health exacerbates sleep issues.
Moreover, the lack of restorative sleep impacts mood regulation. Individuals may find themselves feeling more stressed or overwhelmed in daily situations due to accumulated exhaustion.
Addressing OSA might not only improve physical well-being but could also enhance emotional stability. Treating this condition is crucial for maintaining both mental clarity and overall happiness in life.
Recognizing this link encourages individuals to seek help if they experience symptoms of either condition simultaneously. Understanding that these aspects are interconnected can pave the way for more comprehensive treatment approaches.
Traveling with OSA: Managing Your Condition on the Go
Traveling with obstructive sleep apnea (OSA) can present unique challenges, but preparation is key. First, ensure you have your CPAP machine and accessories packed in carry-on luggage. This guarantees easy access during flights.
Check airline policies regarding medical devices ahead of time. Most airlines allow the use of CPAP machines on board, provided you inform them beforehand.
Bring extra supplies such as hoses, masks, and filters to avoid running out during your trip. Consider a portable power source if you’re traveling to remote areas without reliable electricity.
When booking accommodations, look for hotels that offer rooms equipped with necessary amenities like power outlets near the bed or even designated areas for medical equipment storage.
Maintain a consistent sleep schedule when possible. This helps mitigate OSA symptoms even while away from home. Prioritize rest whenever you can; it’s essential for managing your condition effectively while traveling.
Future Frontiers: Emerging Treatments for Sleep Apnea
The landscape of treatments for Obstructive Sleep Apnea (OSA) is evolving rapidly. Researchers are continuously exploring innovative solutions to improve the quality of life for those affected by this condition. One promising avenue is the development of new devices that offer alternatives to traditional CPAP machines. For instance, advancements in oral appliances have shown great potential in effectively managing OSA symptoms while providing a more comfortable experience.
Another exciting area of research involves neuromodulation techniques, which aim to stimulate certain nerves that control airway function during sleep. This could represent a significant leap forward, offering patients another option beyond conventional therapies.
Additionally, ongoing studies focus on the role of weight loss and lifestyle changes as foundational strategies for treating OSA. With more personalized approaches being explored—like tailored exercise programs and nutritional guidance—the future looks brighter for individuals struggling with this condition.
Genetic research is also paving the way toward understanding why some people are more susceptible to OSA than others. Insights gained from these studies may lead to targeted therapies that address underlying causes rather than just symptoms.
As technology progresses and our understanding deepens, emerging treatments hold promise not only for better management but potentially even cures for obstructive sleep apnea. Staying informed about these developments can empower you or your loved ones on their journey toward improved health and well-being.


