Introduction to Neuromuscular Disorders Affecting Respiration
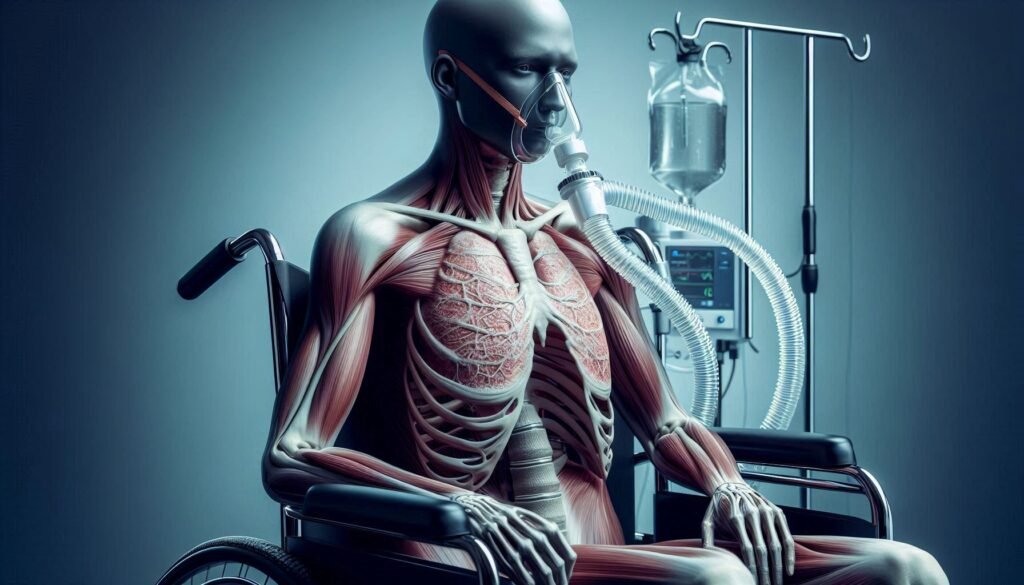
Breathing is an involuntary action that most of us take for granted. Yet, for individuals with neuromuscular disorders, this simple act can become a daunting challenge. Neuromuscular disorders impact the intricate relationship between nerves and muscles, disrupting not only movement but also essential functions like respiration. These conditions affect how our bodies communicate with these vital systems, leading to serious implications for breathing.
Understanding the connection between neuromuscular disorders and respiratory function is crucial. It helps raise awareness about the unique challenges faced by patients and their families while highlighting potential treatments and management strategies available today.
As we dive deeper into this complex topic, we’ll explore various neuromuscular conditions affecting breathing, how they are diagnosed, and innovative therapies being developed to improve quality of life for those affected. Join us on this informative journey as we unravel the intricacies of how nerves and muscles influence one of life’s most fundamental processes: breathing.
The Neuromuscular System: Key Players in Breathing
The neuromuscular system plays a crucial role in breathing. It connects the brain, spinal cord, nerves, and muscles involved in respiration. This intricate network ensures that we can inhale and exhale effortlessly.
“What Causes Pulmonary Hypertension? Understanding High Lung Pressure”
Key players include motor neurons which send signals from the brain to respiratory muscles. The diaphragm is perhaps the most important muscle here. When it contracts, it creates negative pressure in the chest cavity, allowing air to flow into the lungs.
Intercostal muscles also contribute significantly. They are located between the ribs and assist with expanding and contracting the thoracic cavity during breathing cycles.
Any disruption within this system can lead to severe complications in respiratory function. Understanding these components highlights their significance in maintaining healthy breathing patterns.
Common Neuromuscular Disorders Impacting Respiratory Function
Neuromuscular disorders significantly impact respiratory function by affecting the muscles responsible for breathing. Conditions like Amyotrophic Lateral Sclerosis (ALS) and Myasthenia Gravis weaken these essential muscles.
“How Does Cystic Fibrosis Affect Breathing? Complete Guide”
In ALS, motor neurons degenerate over time, leading to muscle atrophy. This progression can severely compromise lung capacity and control of breathing patterns.
Myasthenia Gravis is characterized by muscle fatigue due to disrupted communication between nerves and muscles. Patients may experience weakness in their diaphragm or intercostal muscles, making it challenging to maintain effective ventilation.
Guillain-Barré Syndrome presents another threat with acute onset respiratory failure. The body’s immune system attacks peripheral nerves, resulting in sudden muscle weakness that can extend to those involved in respiration.
“Can Heart Attacks Cause Breathing Problems? Understanding MI”
Muscular dystrophies also contribute to progressive respiratory decline as muscular integrity deteriorates over time. Spinal cord injuries further complicate matters based on the injury level, profoundly influencing a person’s ability to breathe independently.
Amyotrophic Lateral Sclerosis (ALS): Respiratory Challenges and Management
Amyotrophic Lateral Sclerosis (ALS) significantly impacts respiratory function due to its effect on motor neurons. As these neurons degenerate, the muscles responsible for breathing weaken. This can lead to severe respiratory complications.
Patients may experience shortness of breath, especially during physical activities or while lying flat. Eventually, even basic functions like coughing become challenging. Effective management is crucial at this stage.
“What Makes Bronchiectasis Chronic? Treatment Options”
Non-invasive ventilation methods have emerged as lifesavers for many ALS patients. These devices provide support without invasive procedures, improving quality of life substantially.
In more advanced cases, tracheostomy and mechanical ventilation may be necessary to ensure adequate oxygen supply. Close monitoring by healthcare professionals helps tailor treatment strategies effectively.
Regular pulmonary function tests allow physicians to assess lung capacity and monitor disease progression closely. Patients often benefit from a multidisciplinary approach involving neurologists, pulmonologists, and respiratory therapists working together seamlessly.
Myasthenia Gravis: When Breathing Muscles Fatigue
Myasthenia Gravis (MG) is an autoimmune condition that can significantly impact respiratory muscles. In this disorder, the immune system mistakenly attacks the connections between nerves and muscles, leading to weakness. This fatigue can affect various muscle groups, including those necessary for breathing.
“How Do Diaphragm Disorders Affect Breathing? Expert Guide”
Patients may experience shortness of breath or difficulty taking deep breaths due to weakened diaphragm and intercostal muscles. Symptoms often worsen with activity and improve with rest, making daily tasks challenging.
Monitoring respiratory function in MG patients is crucial. As symptoms progress, some individuals might require interventions like non-invasive ventilation during sleep or even invasive support methods if respiratory failure occurs.
Early recognition and management are vital for improving quality of life. Understanding how Myasthenia Gravis affects breathing provides essential insights into patient care and treatment strategies.
Guillain-Barré Syndrome: Acute Respiratory Failure Risks
Guillain-Barré Syndrome (GBS) is an autoimmune disorder that often follows a viral infection. One of the most critical complications associated with GBS is acute respiratory failure.
“What is ALS’s Impact on Breathing? Essential Information”
As the immune system attacks peripheral nerves, muscle strength diminishes rapidly. This weakening can extend to the diaphragm and intercostal muscles, which are essential for effective breathing.
Patients may experience increasing shortness of breath or difficulty in taking deep breaths as the condition progresses. Close monitoring becomes vital in these cases.
Timely intervention can significantly improve outcomes. Healthcare teams may need to initiate non-invasive ventilation or even invasive methods like intubation if respiratory function declines severely.
Recognizing signs early plays a crucial role in managing this risk effectively. Patients and caregivers should remain vigilant about any changes in respiratory status during the course of GBS treatment.
Muscular Dystrophies: Progressive Respiratory Decline
Muscular dystrophies are a group of genetic disorders characterized by progressive muscle weakness and degeneration. As these conditions advance, respiratory function often deteriorates significantly.
“Why Does Platypnea Cause Position-Related Breathing Problems?”
The diaphragm, essential for breathing, can become weakened due to muscle loss. This decline leads to ineffective ventilation and reduced oxygen intake. Patients may experience shortness of breath during exertion or even at rest as the disease progresses.
In addition to direct muscle involvement, scoliosis—a common complication—can further impair lung capacity. The abnormal curvature of the spine restricts chest expansion, making breathing more challenging.
Monitoring respiratory health becomes crucial in managing muscular dystrophies. Regular assessments help identify changes early on and facilitate timely interventions that can improve quality of life for affected individuals. Awareness among caregivers and healthcare providers is vital for ensuring appropriate support and treatment options.
Spinal Cord Injuries: Levels of Injury and Breathing Impact
Spinal cord injuries can significantly impact breathing, depending on the level of injury. Injuries at the cervical level (C1-C8) have profound effects, as they often disrupt signals to the diaphragm and intercostal muscles.
For example, an injury at C4 may result in complete loss of diaphragmatic function. Patients may require ventilatory support due to respiratory muscle paralysis.
Injuries lower in the spinal column, such as those at T1-T12, typically preserve some respiratory function. Individuals might still engage abdominal muscles for forced exhalation but could struggle with deep breaths.
Understanding these levels is crucial for managing care effectively. Each patient’s needs vary based on their specific injury site and severity. Rehabilitation strategies must adapt accordingly to support optimal respiratory health and overall quality of life.
Diagnosing Respiratory Involvement in Neuromuscular Disorders
Diagnosing respiratory involvement in neuromuscular disorders is a critical step in patient management. Early identification can significantly impact treatment decisions and quality of life.
Healthcare providers typically begin with a thorough clinical assessment. They evaluate symptoms such as shortness of breath, cough patterns, and sleep disturbances. Patient history plays a vital role, especially regarding previous diagnoses or familial conditions.
Pulmonary function tests are essential for quantifying respiratory strength. These tests measure lung volumes and airflow rates, helping to determine the extent of impairment.
Additional diagnostic tools may include imaging studies like chest X-rays or CT scans to visualize any structural abnormalities. Blood gas analysis also provides insight into oxygenation levels and carbon dioxide retention.
Close collaboration among neurologists, pulmonologists, and other specialists ensures comprehensive care tailored to each patient’s needs. This multidisciplinary approach enhances diagnosis accuracy and facilitates timely intervention strategies.
Pulmonary Function Tests: Assessing Neuromuscular Respiratory Strength
Pulmonary function tests (PFTs) are essential for evaluating respiratory strength in individuals with neuromuscular disorders. These non-invasive assessments measure how well the lungs and muscles function together.
One common test is spirometry, which gauges airflow during inhalation and exhalation. It provides critical data on lung capacity and can reveal weaknesses in respiratory muscles.
Another important tool is the measurement of maximal inspiratory pressure (MIP). This focuses specifically on the strength of the diaphragm and other breathing muscles. Low MIP values often indicate compromised muscle function due to neuromuscular conditions.
Additionally, body plethysmography helps assess overall lung volume by measuring air trapped within the lungs. This technique offers insights into restrictive or obstructive patterns that may arise from underlying muscular issues.
Regular PFTs can guide treatment decisions and track disease progression, ensuring patients receive optimal care tailored to their specific needs.
Non-Invasive Ventilation: A Game-Changer for Many Patients
Non-invasive ventilation (NIV) has transformed respiratory management for patients with neuromuscular disorders. This technique provides support without the need for invasive procedures like intubation.
NIV aids in improving oxygen levels and reducing carbon dioxide retention. Patients can breathe more easily, often experiencing less discomfort during treatment. Masks or nasal interfaces deliver pressurized air directly to the lungs, allowing for greater patient comfort and autonomy.
The flexibility of NIV is another significant advantage. It can be used at home or in clinical settings, making it accessible to a wide range of individuals facing respiratory challenges due to their conditions.
Moreover, studies show that early intervention with NIV can improve quality of life and prolong survival rates. With ongoing advancements in technology, non-invasive solutions continue to evolve, offering hope to those affected by these debilitating disorders.
Tracheostomy and Mechanical Ventilation: When and Why
Tracheostomy and mechanical ventilation are critical interventions for patients with severe respiratory impairment due to neuromuscular disorders. A tracheostomy involves creating an opening in the neck, allowing direct access to the airway. This procedure is often necessary when conventional intubation is unsuitable or prolonged support is required.
Mechanical ventilation provides breathing assistance by delivering air into the lungs through a ventilator. It can be invasive, using a tube inserted into the trachea, or non-invasive via masks that fit snugly over the face.
These options become essential when respiratory muscles weaken significantly. Patients may experience inadequate oxygen intake or ineffective carbon dioxide removal. Timely intervention helps prevent complications such as respiratory failure and improves quality of life for those affected by conditions like ALS or muscular dystrophies.
Healthcare teams carefully assess each case to determine if these measures are appropriate based on individual needs and prognosis.
Swallowing Disorders and Aspiration Risks in Neuromuscular Conditions
Swallowing disorders, or dysphagia, are common in individuals with neuromuscular conditions. The muscles responsible for swallowing may weaken, making it difficult to safely consume food and liquids.
Aspiration occurs when food or liquid enters the airway instead of the esophagus. This can lead to serious complications like pneumonia. Patients with weakened muscle control are at a heightened risk.
Regular assessments by speech-language pathologists can help identify these challenges early on. They may recommend modified diets or swallowing techniques tailored to individual needs.
Patients should also be educated about the signs of aspiration, such as coughing during meals or changes in voice quality after eating.
By taking proactive measures and ensuring safe eating practices, those affected by neuromuscular disorders can significantly reduce their risks associated with swallowing difficulties.
Chest Physiotherapy and Airway Clearance Techniques
Chest physiotherapy plays a vital role in managing respiratory issues for individuals with neuromuscular disorders. These techniques help maintain lung function and clear secretions that can obstruct airways.
Manual chest physiotherapy includes percussion, vibration, and postural drainage. By using gentle taps on the chest wall, therapists loosen mucus in the lungs. This makes it easier to expel through coughing or suctioning.
Airway clearance devices are increasingly popular as well. These include positive expiratory pressure (PEP) masks and high-frequency oscillation vests. They work by creating vibrations that aid in moving mucus upwards.
Regular sessions of airway clearance not only enhance breathing but also reduce infection risks. For patients facing progressive muscle weakness, these interventions provide essential support to improve quality of life and facilitate better pulmonary health.
Medications Used to Support Respiratory Function
Medications play a crucial role in managing respiratory function for individuals with neuromuscular disorders. These conditions often weaken the muscles responsible for breathing, leading to significant challenges.
Bronchodilators are commonly prescribed to help open airways. They work by relaxing bronchial muscles, making it easier to breathe.
Corticosteroids may also be utilized. These anti-inflammatory drugs can reduce swelling in the airways, improving airflow and overall respiratory efficiency.
For patients experiencing sleep-disordered breathing or severe respiratory insufficiency, non-invasive ventilation support is often recommended. This approach requires careful medication management to ensure optimal comfort and effectiveness during use.
Mucolytics are beneficial as well; they thin mucus secretions, promoting better clearance from the lungs. Maintaining clear air passages is vital for preventing infections.
Supportive therapies like oxygen supplementation can enhance quality of life significantly. Regular monitoring and adjustment of medications ensure that each patient receives personalized care tailored to their unique needs.
Vaccinations and Infection Prevention in Vulnerable Patients
Vaccinations play a crucial role in protecting patients with neuromuscular disorders. These individuals often face respiratory complications due to weakened muscles, making them more susceptible to infections.
Influenza and pneumonia can be particularly dangerous for these patients. Vaccination against these diseases is essential as it helps reduce the risk of severe illness. Regular updates on vaccines are necessary, especially since immunity may wane over time.
In addition to vaccinations, infection prevention strategies should also be prioritized. This includes practicing good hygiene and avoiding crowded places during flu season. Caregivers and family members should also receive vaccinations to minimize exposure risks.
Monitoring for signs of respiratory infections becomes vital in managing health effectively. Early intervention can prevent complications that arise from seemingly minor illnesses, underscoring the importance of proactive care in this vulnerable population.
Psychological Support: Coping with Progressive Respiratory Weakness
Living with neuromuscular disorders can take a toll on mental health, especially as respiratory weakness progresses. Anxiety and depression are common in patients facing the unpredictability of their condition.
Psychological support is crucial for coping mechanisms. Counseling or therapy can provide a safe space to express fears and frustrations. Cognitive-behavioral strategies often help individuals reframe negative thoughts about their situation.
Support groups also play an essential role. Sharing experiences with others who understand the challenges fosters connection and validation. These communities can offer practical advice that resonates personally.
Mindfulness practices, such as meditation or deep-breathing exercises, may alleviate feelings of stress and promote relaxation. Engaging in enjoyable activities can distract from symptoms while enhancing emotional well-being.
Family involvement is key too; educating loved ones about the disorder encourages understanding and patience during challenging times. Together, they create a supportive environment that nurtures resilience amid adversity.
Palliative Care Considerations in Advanced Neuromuscular Disorders
Palliative care plays a crucial role in managing advanced neuromuscular disorders. As these conditions progress, patients often face complex symptoms that require specialized attention.
A multidisciplinary approach is essential. This includes physicians, nurses, social workers, and therapists working together to address physical discomfort and emotional distress. Pain management becomes increasingly important as muscle weakness affects daily activities.
Communication is key in palliative care. Open discussions about goals of treatment help align medical interventions with the patient’s wishes. Advance care planning also ensures that preferences are respected during critical moments.
Support for caregivers cannot be overlooked. They play an integral part in patient care and need resources to manage their own stress and fatigue.
Emotional support should encompass both patients and families alike. Counseling services can provide coping strategies for dealing with the uncertainties of progressive illness while fostering resilience amidst challenges faced by all involved.
Emerging Therapies: From Gene Therapy to Stem Cell Research
Emerging therapies are providing new hope for individuals affected by neuromuscular disorders. Researchers are exploring innovative approaches, including gene therapy and stem cell research, to address the underlying causes of these conditions.
Gene therapy aims to correct genetic defects responsible for certain neuromuscular diseases. By delivering functional copies of genes directly into a patient’s cells, this approach has the potential to halt disease progression or even restore lost functions. Clinical trials have shown promising results in specific conditions like spinal muscular atrophy (SMA).
Stem cell research also holds great promise. Scientists are investigating ways to use stem cells to repair damaged muscles and nerves. These versatile cells can differentiate into various types of tissues, potentially leading to breakthroughs in treating degenerative muscle diseases.
As researchers continue their work, it’s essential for patients and caregivers to stay informed about these advancements. Accessing cutting-edge treatments could significantly improve quality of life and respiratory function for those living with neuromuscular disorders.
The landscape of treatment options is evolving rapidly. With each discovery, there’s renewed optimism that more effective interventions will soon become available for managing respiratory complications associated with these challenging conditions. As we look ahead, collaboration between scientists, healthcare providers, and patient communities remains vital in transforming these emerging therapies into real-world solutions.


