Sarcoidosis is a complex condition that often leaves those affected feeling confused and overwhelmed. It’s more than just a lung disease; it can manifest in various organs, leading to a range of symptoms that vary from person to person. At its core, sarcoidosis involves the formation of tiny clusters of inflammatory cells known as granulomas, which can disrupt normal organ function.
As we delve into this multisystem disorder, we’ll uncover the intricacies of sarcoidosis—from its historical roots to modern-day understanding—and explore how these granulomata transform lives in unexpected ways. Whether you’re seeking knowledge for yourself or supporting someone with this condition, join us on an informative journey through the world of sarcoidosis.
1. What is Sarcoidosis? Understanding the Basics of This Multisystem Disorder
Sarcoidosis is an inflammatory disease characterized by the formation of clusters of immune cells, called granulomas. These small nodules can develop in various organs throughout the body, with the lungs being the most commonly affected site.
This condition often arises without any clear cause and varies significantly from one individual to another. While some people may experience mild symptoms or remain asymptomatic, others could face severe complications requiring medical intervention.
“Why Does Atelectasis Cause Breathing Problems? Understanding Lung Collapse”
The exact mechanisms behind sarcoidosis are still being studied. However, it is believed that genetic factors combined with environmental triggers play a role in its development.
As a multisystem disorder, sarcoidosis can impact not just respiratory health but also skin, eyes, liver, heart, and other vital organs. Recognizing this complexity is essential for understanding how it affects patients’ lives on multiple levels.
2. The History of Sarcoidosis: From Discovery to Modern Understanding
Sarcoidosis was first described in 1877 by the English physician Dr. John Hutchinson. He noted a peculiar skin condition characterized by small, firm nodules. This observation marked the beginning of understanding this complex disease.
“What Makes Pulmonary Fibrosis Progressive? Treatment & Management”
Over the years, researchers began to identify sarcoidosis as not just a dermatological issue but a multisystem disorder, affecting various organs such as the lungs and lymph nodes. The term “sarcoid” was introduced later, emphasizing its granulomatous nature.
In the mid-20th century, advancements in radiology and laboratory techniques allowed for more accurate diagnoses. Researchers uncovered that sarcoidosis is linked to an abnormal immune response.
Today, our understanding continues to evolve with ongoing studies investigating genetic predispositions and potential environmental triggers. As knowledge expands, so does hope for effective treatments tailored to individual patient needs.
3. Causes and Risk Factors: What We Know About Sarcoidosis Development
The exact causes of sarcoidosis remain elusive. Researchers believe a combination of genetic, environmental, and immune factors contribute to its onset.
Certain individuals may have a genetic predisposition that makes them more susceptible to developing this condition. Family history can play a role in increasing risk.
“How Does Myasthenia Gravis Affect Your Breathing? Key Information”
Environmental triggers are another area of interest. Exposure to specific dusts, chemicals, or pathogens could potentially activate an abnormal immune response in vulnerable people.
Age and gender also influence the likelihood of developing sarcoidosis. It is most commonly diagnosed between the ages of 20 and 40 and tends to affect women slightly more than men.
Additionally, some ethnic groups experience higher rates of sarcoidosis; African Americans are notably affected more frequently than Caucasians or Asians. Understanding these risk factors helps illuminate who might be at greater risk for this complex multisystem disorder.
4. Sarcoidosis in Different Organs: Beyond the Lungs
Sarcoidosis is commonly associated with the lungs, but its reach extends to various organs throughout the body. Granulomas can form in places such as the skin, eyes, heart, liver, and lymph nodes.
Skin involvement may manifest as rashes or lesions, often appearing as raised bumps. These changes can be a source of discomfort and self-consciousness for affected individuals.
“What Causes Sudden Dyspnea? Understanding Breathing Difficulties”
The eyes also face risks from sarcoidosis. Uveitis or other inflammatory conditions can lead to vision problems if not addressed promptly. Regular eye examinations are essential for early detection and management.
Cardiac sarcoidosis is particularly concerning due to its potential impact on heart function. It may cause arrhythmias or even heart failure in severe cases.
The liver can become inflamed too but might show no symptoms until advanced stages. Routine monitoring helps in identifying complications early on across all these organ systems.
5. Recognizing Symptoms: The Many Faces of Sarcoidosis
Sarcoidosis can manifest in various ways, making its symptoms quite diverse.
The most common presentation involves the respiratory system. Individuals often experience persistent cough, shortness of breath, and chest pain. However, these signs may be mistaken for other conditions.
Skin involvement is another hallmark feature. Patients may develop rashes or lesions known as erythema nodosum or lupus pernio. These skin changes can vary significantly from person to person.
“Why Is My Breathing So Fast? Understanding Tachypnea”
Eye issues are also prevalent in those with sarcoidosis. Symptoms might include blurred vision, redness, and sensitivity to light—a reminder that this condition doesn’t only affect the lungs.
Fatigue is a pervasive symptom too. Many patients report an overwhelming sense of tiredness that impacts daily activities.
Systemic effects could lead to fevers or weight loss as well. Recognizing these varied symptoms early on plays a crucial role in timely diagnosis and management.
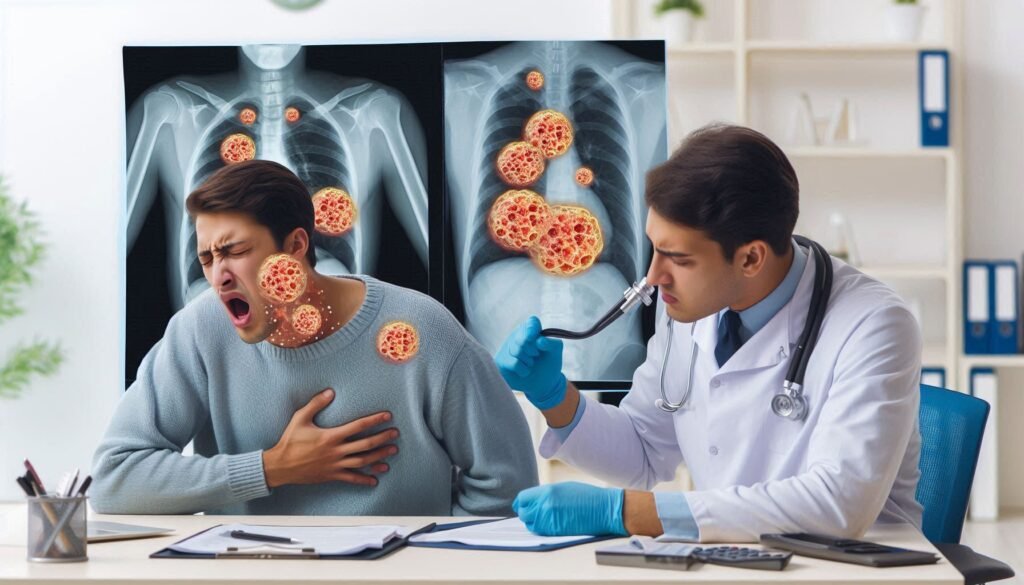
6. Diagnostic Journey: Tests and Procedures to Confirm Sarcoidosis
Diagnosing sarcoidosis can be a complex process. It often begins with a thorough medical history and physical examination. Doctors look for symptoms that suggest inflammation in various organs.
Chest X-rays are commonly used to assess lung involvement. They help identify the characteristic granulomas associated with this condition. However, imaging alone is not definitive.
“What Are the Dangers of Hypoxemia? Signs You Need Medical Help”
A biopsy may be necessary for confirmation. This involves taking a small tissue sample from an affected area, such as the lungs or skin, and examining it under a microscope. Granulomas found in the tissue strongly indicate sarcoidosis.
Blood tests can also play a role in diagnosis by measuring markers of inflammation or organ function impairment. In some cases, additional tests like bronchoscopy or pulmonary function tests are utilized to gather more information about lung capacity and health.
These diverse diagnostic tools ensure accurate identification of sarcoidosis while ruling out other similar conditions.
7. Understanding Granulomas: The Hallmark of Sarcoidosis
Granulomas are small clusters of immune cells that play a crucial role in sarcoidosis. These formations occur as the body responds to perceived threats, such as infections or foreign substances. In sarcoidosis, however, this reaction becomes exaggerated and misdirected.
The hallmark of this condition is the presence of non-caseating granulomas. Unlike caseous lesions found in conditions like tuberculosis, these granulomas do not have central necrosis. Instead, they consist mainly of macrophages surrounded by lymphocytes.
These granulomatous structures can form in various organs throughout the body. While often associated with lung involvement, they may also develop in skin, eyes, liver, and even heart tissues.
Understanding granulomas helps illuminate how sarcoidosis manifests as a multisystem disorder. Their formation reflects an underlying inflammatory process that needs careful management for optimal health outcomes.
8. Treatment Options: Managing Sarcoidosis Symptoms and Progression
Managing sarcoidosis requires a tailored approach, as treatment options can vary widely based on individual symptoms and disease severity. For many patients, the first line of defense includes corticosteroids. These medications help reduce inflammation and manage symptoms effectively.
“How Do Chest Wall Disorders Impact Breathing? Complete Guide”
In cases where corticosteroids are insufficient or cause unwanted side effects, immunosuppressants may be prescribed. Drugs like methotrexate or azathioprine can help control immune response without relying solely on steroids.
Supportive care is also crucial. This might involve physical therapy to enhance lung function or nutritional counseling to address dietary needs.
Regular monitoring is essential for adjusting treatments as needed and ensuring optimal health outcomes. Patients often benefit from multidisciplinary care involving specialists who understand the complexities of this multisystem disorder.
9. Corticosteroids and Immunosuppressants: Key Medications in Sarcoidosis Treatment
Corticosteroids are the cornerstone in managing sarcoidosis. They help reduce inflammation by suppressing the immune response. These medications can significantly alleviate symptoms and prevent complications.
Common corticosteroids include prednisone and methylprednisolone. Doctors often start with a high dose, gradually tapering it down based on patient response. This approach minimizes side effects while effectively managing symptoms.
Immunosuppressants may also be prescribed for those who don’t respond well to corticosteroids or experience severe side effects. Drugs like methotrexate and azathioprine help control the immune system’s activity without relying solely on steroids.
The choice of medication varies depending on individual cases and organ involvement. Regular monitoring is essential to ensure that treatment remains effective while minimizing risks associated with long-term use of these powerful drugs.
10. Living with Sarcoidosis: Lifestyle Adjustments for Better Quality of Life
Living with sarcoidosis often requires making thoughtful lifestyle adjustments. These changes can significantly enhance overall well-being.
Prioritizing rest is essential. Fatigue can be overwhelming, so listening to your body and allowing ample time for recovery is critical.
Adopting a balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports immune function. Staying hydrated also helps maintain energy levels throughout the day.
Regular exercise tailored to personal fitness levels can improve stamina without overexertion. Activities like walking or gentle yoga may promote both physical and mental health.
Additionally, managing stress through relaxation techniques such as meditation or deep-breathing exercises can contribute positively to emotional resilience.
Connecting with support groups provides a sense of community and understanding among those facing similar challenges. Engaging in open conversations about experiences fosters connection while reducing feelings of isolation.
11. Sarcoidosis and the Immune System: Unraveling the Connection
Sarcoidosis is intricately linked to the immune system. At its core, this disorder represents an abnormal response by the body’s immune defenses. Instead of targeting harmful pathogens, the immune system mistakenly attacks healthy tissues.
Granulomas are a hallmark of sarcoidosis and form as a result of this misguided immune reaction. These clusters of inflammatory cells can develop in various organs, disrupting their normal function.
Research suggests that genetic predisposition may play a role in how individuals respond to environmental triggers. Factors like infections or exposure to certain substances might provoke an exaggerated immune response in susceptible individuals.
Understanding this connection between sarcoidosis and the immune system is crucial for developing effective treatments. By targeting specific pathways involved in inflammation, researchers hope to find ways to modulate these responses without compromising overall immunity.
12. Complications of Untreated Sarcoidosis: Why Early Detection Matters
Untreated sarcoidosis can lead to serious complications that affect various organs. The formation of granulomas, while often benign, may obstruct normal organ function over time.
Lung involvement is particularly concerning. Progressive pulmonary sarcoidosis can cause fibrosis, leading to chronic respiratory issues and decreased oxygen levels in the blood. This condition could result in pulmonary hypertension or even respiratory failure.
Beyond the lungs, untreated sarcoidosis might impact the heart. Cardiac sarcoidosis can disrupt electrical signals or weaken heart muscle, increasing the risk of arrhythmias and heart failure.
The eyes are also at risk; untreated cases may lead to vision impairment from conditions like uveitis or glaucoma. Early detection allows for timely intervention, which is crucial in preventing these complications and safeguarding health. Recognizing symptoms promptly plays a vital role in managing this disease effectively.
13. Sarcoidosis in Special Populations: Pregnancy, Children, and the Elderly
Sarcoidosis can affect individuals of any age, including special populations like pregnant women, children, and the elderly. Each group presents unique challenges in terms of management and treatment.
Pregnant women with sarcoidosis may experience changes in their condition due to hormonal fluctuations. It’s crucial for healthcare providers to monitor these patients closely to ensure both maternal and fetal health. Some medications used to manage sarcoidosis may pose risks during pregnancy.
Children diagnosed with sarcoidosis often have a different symptom profile than adults. Early recognition is vital, as pediatric cases can progress rapidly if left untreated. Pediatricians need to be aware of this condition when assessing unexplained symptoms in young patients.
Elderly individuals face additional complications related to comorbidities. Sarcoidosis might mask or mimic other conditions that are common in older adults, complicating diagnosis and treatment plans. A tailored approach is essential for effective care across all demographics affected by this multisystem disorder.
14. Nutrition and Diet: Eating to Support Your Body with Sarcoidosis
Nutrition plays a vital role for those living with sarcoidosis. A balanced diet can help manage symptoms and support overall health.
Focus on whole foods rich in vitamins and minerals. Fruits, vegetables, whole grains, lean proteins, and healthy fats should be staples in your meals. Antioxidant-rich foods like berries can combat inflammation.
Stay hydrated to maintain optimal body function. Water helps flush toxins from the system and supports organ health.
Consider limiting processed foods high in sugar or unhealthy fats. These can trigger inflammation and worsen symptoms over time.
Some individuals may benefit from specific dietary adjustments based on their unique needs. Working with a nutritionist familiar with sarcoidosis can provide personalized guidance.
Listen to your body when it comes to food choices; certain items may cause flare-ups while others might alleviate discomfort. Prioritizing nutrition is an empowering step towards better management of this condition.
15. Exercise and Sarcoidosis: Finding the Right Balance for Your Health
Exercise can be beneficial for individuals with sarcoidosis, but finding the right balance is crucial. Engaging in regular physical activity helps improve lung function and overall stamina. It can also enhance mood and reduce fatigue.
However, it’s essential to listen to your body. Some days may feel more challenging than others due to symptoms like shortness of breath or joint pain. Low-impact exercises such as walking, swimming, or yoga are often recommended because they provide cardiovascular benefits without overwhelming your system.
Consulting a healthcare professional before starting any exercise program is wise. They can help tailor an approach that suits your specific health needs and limitations. Incorporating gentle stretching routines can also aid flexibility and mobility.
Staying active while managing sarcoidosis requires patience and self-awareness. Gradually increasing intensity allows you to gauge how much your body can handle on any given day without pushing beyond its limits.
16. Emotional Impact: Coping with the Uncertainties of Sarcoidosis
Facing a diagnosis of sarcoidosis can be an emotional rollercoaster. Uncertainty about the future often brings anxiety and fear. Patients may find themselves grappling with questions that have no clear answers.
Support from loved ones plays a crucial role during this time. Sharing feelings with family or friends can ease isolation, making it easier to cope with daily challenges. Joining support groups offers a space for connection and understanding among those who share similar experiences.
Mindfulness practices, such as meditation and deep breathing exercises, can help manage stress levels. They provide tools to anchor thoughts in the present moment rather than getting lost in worry about what might come next.
Engaging in creative outlets—like writing or art—can also serve as effective coping mechanisms. These activities allow individuals to express their emotions freely, turning frustration into something constructive and meaningful.
17. Latest Research: New Insights and Promising Treatments for Sarcoidosis
Recent research in sarcoidosis has unveiled exciting insights that could reshape treatment approaches. Scientists are exploring the role of genetic predisposition in developing this condition. Understanding these factors may lead to targeted therapies tailored to individual patients.
Novel treatments have also emerged from clinical trials. For example, medications like abatacept and rituximab show promise for cases resistant to traditional corticosteroids. These agents target different pathways involved in inflammation and immune response.
Additionally, researchers continue investigating biomarkers for early diagnosis and monitoring disease progression. Identifying specific markers can help clinicians predict flares before they manifest clinically.
Another area of focus is the gut microbiome’s influence on sarcoidosis. Studies suggest a link between gut health and systemic inflammation, which could open doors for dietary interventions as complementary therapies.
These advancements bring hope for better management strategies and improved quality of life for those living with sarcoidosis.
18. Sarcoidosis vs. Other Inflammatory Conditions: Differential Diagnosis Challenges
Sarcoidosis presents unique diagnostic challenges due to its overlapping symptoms with other inflammatory conditions. Conditions like rheumatoid arthritis, lupus, and different types of vasculitis often share similar clinical manifestations.
Physicians must carefully evaluate a patient’s medical history and perform comprehensive examinations. This helps distinguish sarcoidosis from these other disorders effectively. Blood tests can provide clues, but results may vary widely among patients.
Imaging studies play a crucial role in the differential diagnosis as well. Chest X-rays or CT scans can reveal characteristic granulomas that are indicative of sarcoidosis but not present in all inflammatory diseases.
In some cases, a biopsy becomes necessary for definitive diagnosis. The presence of noncaseating granulomas is a hallmark sign that helps confirm sarcoidosis over other conditions.
Collaboration among specialists ensures accurate identification and management strategies tailored to each patient’s needs. Misdiagnosis can lead to inappropriate treatments, emphasizing the need for thorough assessment processes.
19. Long-term Outlook: Prognosis and Remission in Sarcoidosis
Understanding the long-term outlook for sarcoidosis is essential for patients and their loved ones. The prognosis varies widely among individuals, with many experiencing a favorable course of the disease while others may face more significant challenges.
For some, sarcoidosis resolves spontaneously within a few months to years without any treatment. These individuals often enter remission and experience no further symptoms or complications. However, about one-third of those affected may develop chronic sarcoidosis that requires ongoing management.
Factors influencing the prognosis include the organs involved and the severity of symptoms at diagnosis. Sarcoidosis primarily affects the lungs but can also impact skin, eyes, heart, and other organs. Patients with pulmonary involvement tend to have better outcomes than those with more extensive systemic effects.
Regular follow-ups are crucial in monitoring disease progression or resolution. Pulmonary function tests can assess lung health over time, while imaging studies help evaluate organ involvement.
Research continues to shed light on potential new treatments that could improve quality of life for those living with this condition. Understanding individual risks factors helps tailor treatment approaches effectively.
Living with sarcoidosis might seem daunting at times; however, many lead productive lives after proper management and support. Creating an open dialogue between patients and healthcare providers fosters understanding and guides effective coping strategies tailored uniquely to each person’s journey through this multifaceted disorder.


