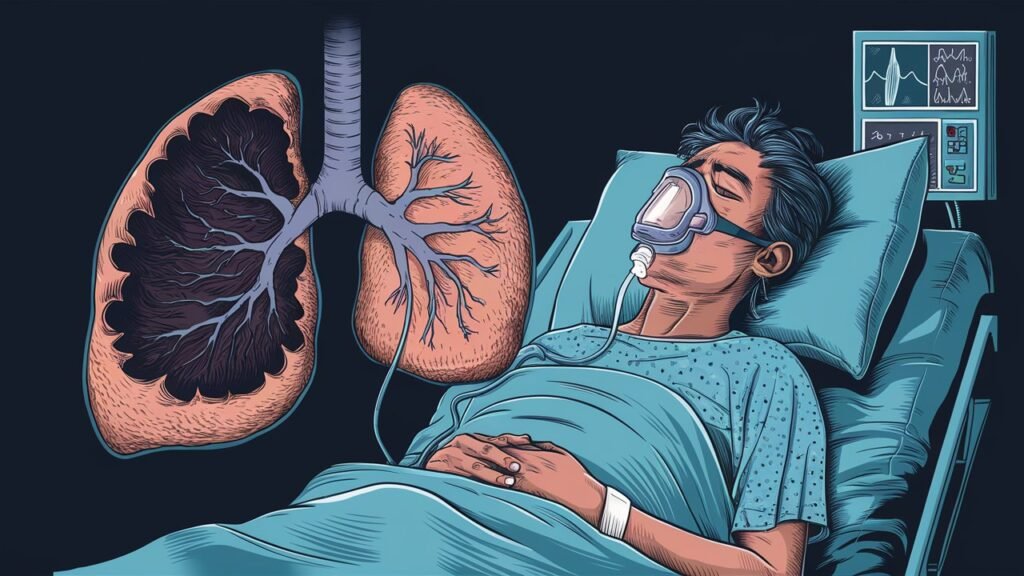
Breathing is something we often take for granted. Each inhale fills our lungs with life-giving oxygen, while each exhale rids us of carbon dioxide. Yet, this delicate process can be disrupted by a condition known as atelectasis. At its core, atelectasis refers to the collapse of lung tissue, which hinders normal airflow and compromises respiratory function.
Understanding how atelectasis affects the body is crucial for recognizing its symptoms and seeking timely treatment. Whether you’re recovering from surgery or managing a chronic illness, knowing more about this condition equips you with valuable insights into maintaining optimal lung health. Let’s dive deeper into how atelectasis disrupts our breathing patterns and what it means for those affected by it.
1. Atelectasis Defined: Unveiling the Collapse of Lung Tissue
Atelectasis is a medical term used to describe the collapse of part or all of a lung. This condition can occur when alveoli, the tiny air sacs in the lungs, become deflated or filled with fluid. As these air spaces lose their ability to hold air, overall lung function diminishes.
The collapse may be partial or complete and can affect one lung more than the other. When atelectasis occurs, it disrupts normal gas exchange, leading to decreased oxygen levels in the bloodstream.
“What Causes Trepopnea? Position-Related Breathing Problems”
Multiple factors contribute to this condition. It can arise from obstructions in the airway due to mucus plugs or tumors. Additionally, external pressure on the lungs—such as from fluid accumulation—can also lead to atelectasis.
Understanding this phenomenon is vital for recognizing its potential impact on health and respiratory efficiency.
2. Lung Anatomy 101: How Atelectasis Disrupts Normal Breathing
The lungs are intricate organs essential for breathing. They consist of millions of tiny air sacs called alveoli, where gas exchange occurs. These structures expand and contract with each breath, allowing oxygen to enter the bloodstream while carbon dioxide is expelled.
“How Does Hypercapnia Affect Your Body? CO2 Buildup Guide”
Atelectasis happens when some or all of these alveoli collapse. This disruption affects airflow and reduces the lung’s overall capacity to function effectively. When sections of the lung are not fully inflated, less surface area is available for oxygen absorption.
As a result, individuals may experience difficulty in maintaining adequate blood oxygen levels. The body compensates by increasing respiratory rate or depth but can struggle if atelectasis persists. Understanding this anatomy helps highlight how crucial it is to keep lung tissue healthy and functioning optimally for normal breathing patterns.
3. Types of Atelectasis: From Obstructive to Compressive
Atelectasis comes in several forms, each impacting lung function differently. Understanding these types is crucial for effective management.
“What Causes Respiratory Acidosis? Complete Treatment Guide”
Obstructive atelectasis occurs when air passages are blocked, preventing air from reaching parts of the lungs. This blockage can result from mucus plugs, tumors, or foreign objects. The affected tissue collapses due to a lack of air.
Compressive atelectasis happens when external pressure causes lung collapse. Conditions like pleural effusion—where fluid accumulates between the layers surrounding the lungs—can lead to this type. Tumors pressing on the lung can also create similar effects.
Other variations include adhesive atelectasis and contraction atelectasis. Adhesive refers to alveoli sticking together due to insufficient surfactant production, while contraction involves scarring that alters normal lung structure.
“How Serious is Hypoventilation Syndrome? Warning Signs”
Recognizing these distinctions aids healthcare providers in tailoring treatment strategies effectively.
4. Common Causes: Surgery, Bed Rest, and Other Risk Factors
Atelectasis can arise from various factors, with certain conditions increasing its likelihood. Surgery is a prominent cause, particularly procedures involving the chest and abdomen. Anesthesia can suppress breathing patterns, leading to lung collapse.
“What Makes Aspiration Dangerous? Prevention & Treatment”
Prolonged bed rest is another significant risk factor. Staying immobile reduces lung expansion and may allow air sacs to deflate. This is especially common in patients recovering from surgery or those with chronic illnesses.
Other underlying issues like mucus buildup due to respiratory infections also contribute to atelectasis. Blockages prevent airflow into parts of the lungs, causing them to collapse over time.
Certain lifestyle choices can exacerbate these risks as well. Smoking impairs lung function and increases susceptibility to respiratory complications that could lead to atelectasis. Environmental factors such as pollution may further compromise lung health, creating unfavorable conditions for adequate breathing.
5. Symptoms Deep Dive: Beyond Shortness of Breath
Atelectasis manifests in various ways, extending beyond the commonly recognized symptom of shortness of breath. Patients may experience a persistent cough as the body attempts to clear secretions from collapsed lung areas.
“Why Does Bronchospasm Happen? Triggers & Solutions”
Chest pain can also occur, often due to pressure changes within the lungs or irritation of surrounding tissues. This discomfort might be sharp or dull and can worsen with deep breaths or coughing.
Fatigue is another notable symptom. Reduced oxygen levels caused by atelectasis lead to feelings of exhaustion and decreased energy for daily activities.
In more severe cases, cyanosis—bluish discoloration of lips and fingertips—may develop. This indicates inadequate oxygen supply and requires immediate medical attention.
“What Causes Metabolic Acidosis? Impact on Breathing”
Recognizing these symptoms early is crucial for effective management and recovery from atelectasis-related complications. Awareness empowers individuals to seek timely care when needed.
6. Acute vs Chronic Atelectasis: Understanding the Differences
Acute atelectasis occurs suddenly, often triggered by an event such as surgery or a severe respiratory infection. It can lead to rapid changes in lung function and may require immediate medical intervention. Symptoms include sudden shortness of breath and chest pain.
Chronic atelectasis, on the other hand, develops gradually over time. It is typically linked to underlying conditions like cystic fibrosis or chronic obstructive pulmonary disease (COPD). Patients may experience progressive symptoms that are less intense but persist longer.
“How Serious is ARDS? Understanding Acute Respiratory Distress”
Understanding these differences is crucial for effective management. Acute cases might resolve quickly with treatment, while chronic forms demand ongoing monitoring and care strategies tailored to the patient’s specific needs. Each type presents unique challenges in maintaining optimal lung function and overall health.
7. Diagnostic Techniques: X-rays, CT Scans, and Bronchoscopy
Diagnostic techniques play a crucial role in identifying atelectasis. Among the most common methods are X-rays, CT scans, and bronchoscopy.
X-rays provide a quick overview of lung structures. They can reveal areas of collapsed lung tissue but may not show the complete picture.
“What Makes Obstructive Sleep Apnea Different? Complete Guide”
CT scans offer more detailed images. This imaging technique allows healthcare providers to assess the extent and location of atelectasis with precision, helping guide treatment decisions effectively.
Bronchoscopy is another valuable tool. It involves inserting a thin tube into the airways to visualize them directly. This method can help identify blockages or other abnormalities contributing to lung collapse.
Each diagnostic method has its strengths and limitations. Choosing the right one depends on individual patient circumstances and clinical judgment. Proper diagnosis is essential for effective management of atelectasis, ensuring timely intervention for better outcomes.
8. Treatment Strategies: Addressing the Root Cause of Atelectasis
Addressing atelectasis involves identifying and treating its underlying causes. This tailored approach is crucial for effective management.
If airway obstruction is the issue, options like bronchoscopy may be employed to remove blockages. Clearing mucus or foreign bodies can restore lung function quickly.
For individuals recovering from surgery, deep breathing exercises play a vital role. Encouraging regular inhalation helps keep airways open and prevents further collapse.
“Could It Be Mesothelioma? Early Warning Signs & Risk Factors”
Patients who are bedridden benefit significantly from incentive spirometry. This device encourages deeper breaths, enhancing lung expansion over time.
In some cases, addressing environmental factors such as smoking cessation or exposure to pollutants can also prove beneficial.
Medication may be warranted for those with underlying conditions like asthma or COPD that contribute to atelectasis. Bronchodilators help ease airflow and improve overall respiratory health.
Personalized treatment plans focusing on the root cause foster better recovery outcomes in patients dealing with this condition.
9. Respiratory Therapy: Techniques to Re-expand Collapsed Lung Tissue
Respiratory therapy is pivotal in managing atelectasis. It employs several techniques aimed at re-expanding collapsed lung tissue. One common method is deep breathing exercises, which encourage lung expansion and improve airflow.
Incentive spirometry plays a crucial role as well. This device motivates patients to take slow, deep breaths while keeping a visual indicator within a target range. Regular use can significantly enhance lung function over time.
Positive expiratory pressure (PEP) therapy is another effective technique. By creating resistance during exhalation, PEP helps open airways and promotes mucus clearance from the lungs.
Chest physiotherapy involves manual techniques that help loosen secretions in the lungs, making it easier for patients to breathe deeply again. Each of these methods is tailored to individual needs, ensuring optimal recovery from atelectasis-related challenges.
10. Incentive Spirometry: A Key Tool in Atelectasis Prevention and Treatment
Incentive spirometry is an essential method used to prevent and treat atelectasis. This device encourages deep breathing, which helps keep the alveoli open. By taking slow, deep breaths, patients can improve lung expansion and increase oxygen intake.
Using an incentive spirometer is simple. A patient inhales slowly through a mouthpiece while watching a gauge rise. The goal is to reach a designated target that indicates proper lung inflation. Regular use promotes better respiratory function.
Healthcare providers often recommend this tool for patients recovering from surgery or those on prolonged bed rest. Consistent practice not only enhances airflow but also reduces the risk of complications such as pneumonia.
Patients should be encouraged to incorporate incentive spirometry into their daily routines, especially in high-risk scenarios. Personalizing goals based on individual capacity can further motivate adherence and success in treatment outcomes.
11. Postural Drainage: Positioning for Better Lung Function
Postural drainage is a therapeutic technique aimed at promoting better lung function. It involves positioning the body in specific ways to facilitate mucus clearance from the lungs.
By utilizing gravity, postural drainage helps move secretions toward larger airways where they can be coughed out more effectively. It’s particularly beneficial for individuals with atelectasis or other respiratory conditions that lead to mucus accumulation.
Different positions target various lobes of the lungs. For instance, lying on one side may help drain fluid from a particular lung section. In contrast, sitting upright can aid overall lung expansion and airflow.
Incorporating this technique into daily routines can significantly enhance respiratory health. Patients should work closely with healthcare professionals to establish effective positioning strategies tailored to their individual needs and conditions.
12. Medications in Atelectasis Management: Bronchodilators and Beyond
Managing atelectasis often involves a combination of therapies, including medications. Bronchodilators play a crucial role in this process. These drugs help to open the airways, allowing for improved airflow and easier breathing.
By reducing bronchospasm, bronchodilators can alleviate some symptoms associated with lung collapse. They are particularly beneficial for individuals who have underlying conditions like asthma or chronic obstructive pulmonary disease (COPD).
In addition to bronchodilators, corticosteroids may be prescribed to reduce inflammation within the airways. This can enhance overall lung function and promote better oxygen exchange.
Expectorants are also sometimes utilized. They assist in thinning mucus secretions, making it easier for patients to clear their lungs through coughing.
These medications empower healthcare providers to tailor treatment plans based on individual needs while addressing the varying causes and effects of atelectasis effectively.
13. Surgical Interventions: When Conservative Treatments Fail
Surgical interventions become necessary when conservative treatments for atelectasis fail to yield results. In some cases, breathing exercises or medications may not be enough to re-expand the collapsed lung tissue.
One common surgical approach is bronchoscopy. This procedure allows physicians to remove obstructions blocking airways, such as mucus plugs or foreign bodies. By clearing these blockages, normal airflow can be restored.
Another option is lobectomy or wedge resection for those with significant scarring or damage in a specific lung area. Such surgeries involve removing a portion of the affected lung and can improve overall respiratory function.
In severe scenarios where other treatments are ineffective, thoracotomy may be required. This invasive surgery provides direct access to the lungs and pleural space, enabling more extensive interventions.
Patient selection is crucial before opting for surgery. Factors like overall health and underlying conditions significantly influence outcomes following any surgical intervention related to atelectasis.
14. Preventing Atelectasis: Strategies for High-Risk Individuals
Preventing atelectasis is crucial, especially for those at high risk. Strategies can significantly improve lung health and function.
Encouraging mobility is one of the most effective methods. Patients should be motivated to move around whenever possible. Simple activities like sitting up or walking can stimulate deep breathing and help prevent lung tissue collapse.
Incentive spirometry plays a vital role as well. This device encourages patients to take deep breaths by providing visual feedback on their inhalation efforts. Regular use promotes alveolar expansion, reducing the chances of atelectasis.
Proper positioning also matters. Elevating the head of the bed can enhance lung ventilation, particularly in postoperative patients or those with limited mobility.
Another important factor is hydration. Keeping mucus thin helps maintain airway patency and facilitates coughing out secretions that could contribute to blockage.
Educating caregivers about identifying early signs of respiratory distress ensures timely intervention when necessary.
15. Atelectasis in Critical Care: Managing Ventilated Patients
Atelectasis poses a significant challenge in critical care settings, particularly among ventilated patients. The risk of lung collapse increases due to prolonged mechanical ventilation and sedation, which can inhibit normal breathing patterns.
In these cases, regular assessments are crucial. Monitoring lung sounds and oxygen saturation helps identify early signs of atelectasis. Techniques such as repositioning the patient frequently can enhance lung expansion and prevent further complications.
Implementing positive end-expiratory pressure (PEEP) on ventilators is another effective strategy. PEEP keeps alveoli open at the end of expiration, minimizing the risk of collapse.
Respiratory therapists play an essential role in this environment. They may employ various methods like deep breathing exercises or incentive spirometry to promote better ventilation.
Education for nursing staff about recognizing potential atelectasis is vital in managing high-risk patients effectively. Taking proactive measures ensures that vulnerable individuals receive timely interventions to maintain optimal respiratory function.
16. Pediatric Atelectasis: Special Considerations for Young Patients
Pediatric atelectasis presents unique challenges. Children, especially infants, have smaller lung volumes and less muscle strength. This makes them more susceptible to lung collapse.
Anatomical differences play a role as well. The airways in younger patients are narrower and more easily obstructed by mucus or foreign objects. These factors can lead to rapid deterioration in respiratory function.
Symptoms may also differ from adults. Young children might exhibit irritability or feeding difficulties rather than typical signs like shortness of breath. Parents should be vigilant for any unusual behaviors that could indicate breathing issues.
Treatment must be tailored for pediatric patients, focusing on gentle interventions. Techniques such as incentive spirometry can be adapted for age-appropriate use, helping young ones learn deep breathing without stress.
Monitoring is critical during recovery since children’s conditions can change quickly. Regular follow-ups ensure that any complications are addressed promptly to support healthy lung development.
17. Complications of Untreated Atelectasis: From Pneumonia to Respiratory Failure
Untreated atelectasis can lead to a cascade of complications that significantly impact respiratory health. One of the most common issues is pneumonia. When lung tissue collapses, it creates an environment conducive to bacterial growth, increasing the risk of infection.
Additionally, atelectasis can cause hypoxemia, a condition where oxygen levels in the blood drop dangerously low. This places strain on vital organs and systems throughout the body.
In severe cases, persistent atelectasis may progress to respiratory failure. The lungs struggle to provide adequate oxygenation and remove carbon dioxide effectively. Patients may experience extreme fatigue and confusion due to insufficient oxygen supply.
Moreover, untreated atelectasis can contribute to chronic lung disease over time. Recurrent episodes exacerbate existing conditions like asthma or COPD, leading to further decline in lung function.
Understanding these potential complications emphasizes the importance of timely intervention for individuals affected by this condition.
18. Recovery Timeline: What to Expect After Atelectasis Treatment
After treatment for atelectasis, the recovery timeline can vary significantly among individuals. Factors such as the underlying cause, treatment method, and overall health play crucial roles in determining how quickly one heals.
Initially, patients may experience shortness of breath or mild discomfort as lung function begins to improve. This phase usually lasts a few days to weeks post-treatment. Breathing exercises and respiratory therapy are often recommended during this period to help restore lung capacity.
As healing progresses, most individuals see gradual improvements in their symptoms. Follow-up appointments with healthcare providers are essential for monitoring progress and adjusting treatment plans if necessary.
For some people, full recovery can take several weeks or even months. Adhering strictly to prescribed therapies is vital for optimal outcomes and minimizing the risk of recurrence in the future. Regular check-ins will help ensure that any lingering issues are addressed promptly.
19. Long-term Outlook: Living with Recurrent Atelectasis
Living with recurrent atelectasis can be challenging. Individuals may experience frequent episodes that disrupt their daily activities and overall well-being. Understanding the condition is crucial for effective management.
Monitoring lung health becomes essential. Regular check-ups allow healthcare providers to track changes in lung function and intervene early when necessary. This proactive approach helps mitigate complications, such as pneumonia or respiratory failure.
Lifestyle modifications play a significant role too. Maintaining good hydration, practicing deep breathing exercises, and avoiding smoking can improve lung capacity and reduce recurrence risk.
Patients should also stay informed about their treatment options, including medications or therapies that help keep airways open. Open communication with healthcare professionals enhances understanding of personal triggers and strategies tailored to individual needs.
Support groups may provide emotional relief by connecting individuals facing similar challenges. Sharing experiences fosters resilience against the uncertainties of living with recurrent atelectasis.
20. Emerging Research: New Approaches to Atelectasis Prevention and Treatment
Emerging research is paving the way for innovative approaches in both the prevention and treatment of atelectasis. Scientists are exploring novel therapies that target not just symptoms but also underlying causes. This includes advances in drug formulations aimed at improving lung function, enhancing surfactant replacement therapies, and developing biomaterials that promote lung tissue repair.
Additionally, studies are focusing on individualized patient care strategies. Personalized treatment plans based on genetic profiling or specific risk assessments may improve outcomes significantly. Researchers are also investigating the role of advanced imaging techniques to better understand how atelectasis develops and progresses in different populations.
Moreover, technology is making strides with wearable devices capable of monitoring respiratory patterns continuously. These tools could alert patients and healthcare providers early on about changes that might indicate an increased risk for collapse.
As we delve deeper into understanding atelectasis, these advancements hold promise for more effective management strategies tailored to individual needs while reducing hospital stays and complications associated with this condition. The future looks hopeful as medical science continues its quest to enhance lung health and overall quality of life through targeted interventions against atelectasis.


