Amyotrophic Lateral Sclerosis (ALS) is a progressive neurological disease that presents unique challenges for those diagnosed and their families. Often characterized by the degeneration of motor neurons, ALS affects voluntary muscle movements, leading to difficulties in speaking, swallowing, and ultimately breathing. The impact on respiratory function can be particularly distressing as breathing becomes increasingly labored over time.
Understanding ALS requires delving into its complex nature and recognizing how it not only disrupts physical capabilities but also creates emotional turmoil for patients. While the early signs may start subtly—perhaps a slight weakness or fatigue—the eventual progression can lead to significant complications like trouble breathing. This blog post will explore various facets of ALS: from its neuropathology and types to diagnostic methods and treatment approaches designed to manage symptoms effectively.
Join us as we unravel the intricacies of this challenging condition, shedding light on ways to navigate its many hurdles while focusing on quality of life for both patients and caregivers alike.
1. ALS Unveiled: Understanding the Progressive Nature of Motor Neuron Degeneration
Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disorder that primarily affects motor neurons in the brain and spinal cord. These specialized cells are responsible for transmitting signals from the nervous system to voluntary muscles. As ALS progresses, these neurons gradually deteriorate and die.
The result is a steady decline in muscle control and strength, leading to significant physical challenges. Individuals may experience difficulties with everyday tasks such as walking or holding objects.
“Why Does Bronchospasm Happen? Triggers & Solutions”
What makes ALS particularly insidious is its unpredictable progression; symptoms can vary greatly between individuals. Some may notice rapid declines, while others experience slower degeneration over years. This variability adds complexity not only to diagnosis but also to management strategies.
Understanding this progressive nature of ALS helps patients and families prepare for future changes in health status, emphasizing the need for ongoing support throughout their journey.
2. The Neuropathology of ALS: How It Affects Breathing and Muscle Function
Amyotrophic Lateral Sclerosis (ALS) is characterized by the degeneration of motor neurons in the brain and spinal cord. These essential cells are responsible for voluntary muscle movements, including those involved in breathing.
“What Causes Metabolic Acidosis? Impact on Breathing”
As motor neurons deteriorate, communication between the nervous system and muscles becomes impaired. This leads to weakness and atrophy of respiratory muscles such as the diaphragm and intercostal muscles.
When these muscles weaken, effective lung function decreases. Patients may experience shortness of breath or fatigue during everyday activities. The inability to take deep breaths can also impact coughing reflexes, making it difficult to clear secretions from the lungs.
With time, this deterioration can result in serious complications related to breathing difficulties. Managing these symptoms becomes crucial for maintaining quality of life as ALS progresses. Understanding this aspect helps caregivers anticipate needs better.
3. Types of ALS: Sporadic vs. Familial Forms
Amyotrophic Lateral Sclerosis (ALS) primarily manifests in two forms: sporadic and familial.
Sporadic ALS is the most common type, accounting for approximately 90-95% of all cases. It typically arises without a known genetic cause and generally affects individuals later in life, around their mid-50s to early 60s. The exact triggers remain elusive, although environmental factors may contribute.
“How Serious is ARDS? Understanding Acute Respiratory Distress”
Familial ALS, on the other hand, has a clear genetic link. This form occurs when mutations are inherited from one or both parents. Familial ALS accounts for about 5-10% of cases and often presents at an earlier age compared to its sporadic counterpart.
Understanding these distinctions aids in diagnosis and treatment approaches while highlighting the complex nature of this neurodegenerative disease. Each type requires tailored management strategies based on individual needs and family history.
4. Early Signs of ALS: From Muscle Weakness to Subtle Breathing Changes
Early signs of Amyotrophic Lateral Sclerosis (ALS) can be subtle, often making diagnosis challenging. One of the first symptoms is muscle weakness. Individuals may notice difficulty with tasks that once seemed effortless, like buttoning a shirt or climbing stairs.
“What Makes Obstructive Sleep Apnea Different? Complete Guide”
As the disease progresses, changes in breathing patterns may emerge. Patients might experience shortness of breath during physical activities they previously managed without issue. This symptom can easily go overlooked.
Another early indicator includes muscle cramps and twitching, known as fasciculations. These sensations occur when motor neurons begin to degenerate but are not always recognized as significant warning signs.
Moreover, some individuals report fatigue that doesn’t align with their activity levels. This overwhelming tiredness combined with emerging respiratory issues demands attention and further evaluation by healthcare professionals to explore potential underlying causes such as ALS.
5. The Progression of ALS: Respiratory Involvement and Disease Milestones
The progression of Amyotrophic Lateral Sclerosis (ALS) varies significantly among individuals. One common aspect is the gradual decline in respiratory function. As motor neurons degenerate, the muscles responsible for breathing weaken.
“Could It Be Mesothelioma? Early Warning Signs & Risk Factors”
Initially, patients may experience mild difficulty during physical exertion or sleep. This can manifest as shortness of breath after simple activities or increased fatigue at night.
As ALS advances, respiratory involvement becomes more pronounced. Patients often find it challenging to take deep breaths or cough effectively. In some cases, they might develop a condition known as hypoventilation due to weakened diaphragm muscles.
Disease milestones vary but typically include significant changes in lung capacity and reliance on assistive devices for breathing support. Monitoring these changes is crucial for effective management and intervention strategies throughout the disease course.
6. Diagnosing ALS: The Complex Journey to a Definitive Answer
Diagnosing Amyotrophic Lateral Sclerosis (ALS) can be a challenging process. There is no single test that definitively confirms the disease. Instead, healthcare providers follow a series of steps to rule out other conditions.
Initially, they conduct a comprehensive medical history review and physical examination. This helps identify symptoms such as muscle weakness or coordination issues. Since these signs may overlap with other diseases, neurologists often rely on specific tests.
“Why Does Breathing Worsen at Night? Understanding PND”
Advanced imaging techniques like MRI scans can help visualize brain and spinal cord changes. Blood tests are also critical in excluding various inflammatory or infectious diseases.
Electromyography (EMG) plays a crucial role in the diagnostic journey by assessing electrical activity in muscles. Abnormal results from EMG studies provide valuable insights into motor neuron health.
Collaboration among specialists enhances accuracy in diagnosis, ensuring patients receive appropriate care tailored to their needs.
7. Electromyography and Nerve Conduction Studies: Key Diagnostic Tools
Electromyography (EMG) and nerve conduction studies (NCS) play crucial roles in diagnosing Amyotrophic Lateral Sclerosis (ALS). These tests help evaluate the electrical activity of muscles and the speed at which nerves transmit signals.
During an EMG, a thin needle electrode is inserted into specific muscles. This allows doctors to assess muscle response when stimulated by nerve impulses. Abnormal results often indicate damage or degeneration, a hallmark of ALS.
“What Are the Early Warning Signs of Asthma? Complete Guide”
Nerve conduction studies measure how quickly electrical signals travel through peripheral nerves. By stimulating nerves with small pulses and recording their responses, clinicians can identify areas of dysfunction.
Together, these diagnostic tools provide essential insights into motor neuron health. They aid in differentiating ALS from other neuromuscular disorders that may present similar symptoms. The precision offered by EMG and NCS is invaluable for patients on their journey toward understanding their condition better.
8. Genetic Testing in ALS: Implications for Patients and Families
Genetic testing plays a crucial role in understanding Amyotrophic Lateral Sclerosis (ALS), particularly in deciphering its familial forms. By identifying specific gene mutations, healthcare providers can determine an individual’s risk of developing ALS.
“How Does Congestive Heart Failure Affect Your Breathing? Key Signs”
For patients and families, the implications can be profound. Positive results may lead to increased surveillance for symptoms and proactive management strategies. Knowing one’s genetic status allows for informed decision-making regarding family planning and lifestyle changes.
Moreover, genetic insights pave the way for targeted therapies tailored to specific mutations. As research advances, potential treatments could directly address these underlying causes of ALS.
However, the emotional weight of genetic testing cannot be overlooked. Patients and families often face tough conversations about inheritance patterns and future health risks. Support from professionals is essential to navigate these complexities effectively.
9. Respiratory Function Tests: Monitoring Lung Capacity in ALS
Monitoring lung capacity is crucial for individuals with Amyotrophic Lateral Sclerosis (ALS). As motor neurons degenerate, the muscles responsible for breathing weaken. This can lead to significant respiratory complications.
“Can Anemia Cause Shortness of Breath? Understanding the Connection”
Respiratory function tests are essential in assessing lung health. These tests measure various aspects of breathing, including forced vital capacity (FVC), which gauges how much air a person can exhale after taking a deep breath. A decline in FVC may indicate respiratory muscle weakness.
Spirometry is a common tool used during these assessments. It provides valuable insights into airflow and volume changes over time. Regular testing helps track disease progression and informs treatment decisions.
Early detection of respiratory issues allows healthcare providers to implement timely interventions. Strategies may include breathing exercises or mechanical ventilation support as needed to improve quality of life for ALS patients facing trouble breathing.
10. Treatment Approaches: Managing Symptoms and Slowing Progression
Managing symptoms of Amyotrophic Lateral Sclerosis (ALS) is crucial for improving quality of life. Treatment approaches are tailored to individual needs, focusing on symptom relief and prolonging mobility.
Medications such as Riluzole can help slow disease progression by decreasing glutamate levels in the brain. Edaravone has also shown promise in reducing oxidative stress associated with ALS.
Physical therapy plays a vital role. Tailored exercise regimens preserve muscle strength and flexibility while preventing stiffness. Occupational therapy helps adapt daily activities, ensuring independence for as long as possible.
Speech therapy becomes essential when communication challenges arise. Techniques taught by therapists can improve speech clarity or offer alternative methods like text-to-speech devices.
Nutritional support cannot be overlooked either. Proper diet management addresses swallowing difficulties and maintains energy levels, which is critical for overall health during the progression of ALS.
11. FDA-Approved Medications for ALS: Understanding Their Mechanisms and Effects
Several FDA-approved medications aim to manage Amyotrophic Lateral Sclerosis (ALS) symptoms and potentially slow disease progression. Riluzole, the first medication approved for ALS in 1995, works by inhibiting glutamate release. This action reduces excitotoxicity, a harmful process that can damage motor neurons.
Another significant drug is edaravone, introduced in 2017. It functions as an antioxidant, scavenging free radicals that contribute to cellular damage. Clinical trials have shown it may help preserve physical function over time.
Additionally, Nuedexta combines two existing drugs to address pseudobulbar affect—a condition characterized by uncontrollable laughter or crying often seen in ALS patients. By modulating neurotransmitter activity in the brain, it helps improve emotional stability.
These medications offer varying benefits but do not cure ALS. They represent critical steps toward enhancing patient care and quality of life amid ongoing research into more effective treatments.
12. Respiratory Support in ALS: From Assisted Ventilation to Tracheostomy
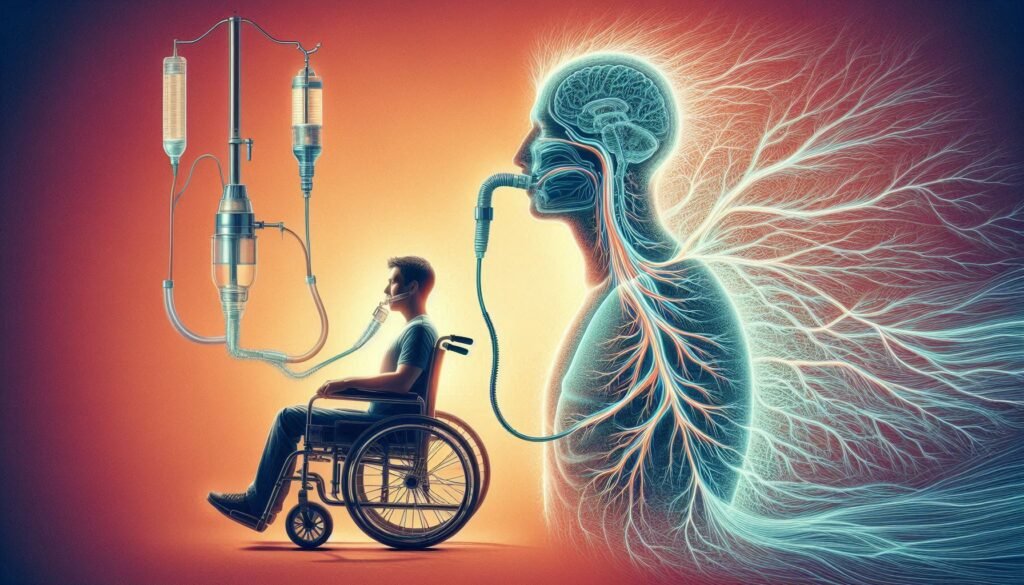
Respiratory support is essential for individuals with Amyotrophic Lateral Sclerosis (ALS) as the disease progresses. Breathing difficulties often emerge due to weakened respiratory muscles, making it challenging for patients to maintain adequate oxygen levels.
Assisted ventilation can provide significant relief. Devices like BiPAP machines help by delivering air through a mask during sleep or when needed throughout the day. This non-invasive option allows patients to breathe more comfortably without invasive procedures.
In cases where assistance becomes critical, tracheostomy might be considered. This surgical procedure involves creating an opening in the neck to insert a tube directly into the windpipe. It provides a reliable airway and can facilitate long-term ventilation support.
Each patient’s needs are unique, requiring careful evaluation and personalized care plans tailored to their specific condition and preferences. Respiratory interventions aim not only to enhance breathing but also improve overall quality of life for those living with ALS.
13. Nutritional Management: Addressing Swallowing Difficulties and Maintaining Weight
Nutritional management is crucial for individuals with Amyotrophic Lateral Sclerosis (ALS) as the disease often leads to swallowing difficulties. Dysphagia can make it challenging to consume adequate nutrition, resulting in weight loss and malnutrition.
Soft foods and pureed diets may be necessary to facilitate easier swallowing. Foods high in calories and protein become essential for maintaining strength and energy levels. Smoothies, nutritional shakes, and fortified foods can help meet dietary needs without overwhelming the individual.
Regular assessments by healthcare professionals ensure that dietary adjustments are made according to changing abilities. Speech-language pathologists play a key role in recommending appropriate textures and strategies for safe eating.
Patients might also benefit from adaptive utensils designed specifically for those with limited hand function. Staying hydrated is vital; however, thickening agents may sometimes be added to liquids to prevent choking hazards during drinking sessions.
14. Physical Therapy and Exercise in ALS: Preserving Function and Quality of Life
Physical therapy plays a crucial role in the management of Amyotrophic Lateral Sclerosis (ALS). It focuses on maintaining mobility and function as muscle strength declines. Tailored exercise programs aim to enhance endurance without overexertion.
Gentle stretching can help maintain flexibility, reducing stiffness and discomfort. Occupational therapists often join forces with physical therapists to adapt daily activities, ensuring independence for as long as possible.
Assistive devices may be introduced to facilitate movement and safety at home. These tools greatly improve quality of life by allowing individuals to engage more fully in their surroundings.
Group sessions or community classes foster social interaction, which is vital for emotional well-being. Connecting with others facing similar challenges offers support and encouragement throughout the journey with ALS.
Regular evaluation ensures that therapies evolve alongside changing needs, helping patients navigate this progressive condition effectively while preserving dignity and enjoyment in life’s simple moments.
15. Speech and Communication Challenges: Adaptive Technologies and Strategies
As Amyotrophic Lateral Sclerosis (ALS) progresses, individuals often face significant speech and communication challenges. The weakening of the muscles involved in speaking can make it difficult to articulate words clearly.
Adaptive technologies play a crucial role in facilitating communication for those affected by ALS. Speech-generating devices allow users to communicate through synthesized voices or text-to-speech applications, enhancing their ability to express thoughts and needs effectively.
Augmentative and alternative communication (AAC) methods are also valuable. These can include picture boards or eye-tracking systems that translate eye movements into speech, ensuring patients maintain a voice even as physical capabilities diminish.
Support from speech-language pathologists is vital too. They provide tailored strategies to maximize remaining abilities and recommend appropriate technology options based on individual needs.
16. Palliative Care in ALS: Enhancing Comfort and Quality of Life
Palliative care plays a crucial role in the management of Amyotrophic Lateral Sclerosis (ALS). It focuses on improving comfort and enhancing quality of life for patients facing this progressive disease.
This specialized form of care addresses not only physical symptoms but also emotional, spiritual, and social needs. By providing comprehensive support, healthcare professionals can help alleviate pain and discomfort associated with ALS.
A multidisciplinary approach is often employed, involving doctors, nurses, psychologists, and therapists. Together they create personalized plans that prioritize patient preferences.
Communication is vital in palliative care. Engaging discussions about goals and desires empower patients to make informed decisions regarding their treatment options.
Support extends beyond the individual; families benefit greatly from resources aimed at navigating the challenges posed by ALS. With education and guidance from experienced providers, loved ones can feel more equipped to support their family member during this difficult journey.
17. Psychological Support: Coping with the Emotional Impact of ALS
The emotional toll of Amyotrophic Lateral Sclerosis (ALS) is profound. Patients often grapple with feelings of anxiety, sadness, and isolation as they navigate the disease’s challenges.
Psychological support plays a vital role in coping with these emotions. Therapists trained in chronic illness can provide essential strategies tailored to individual needs. Cognitive-behavioral therapy, for instance, helps patients reframe negative thoughts into more positive ones.
Support groups also offer a community where individuals share their experiences and feelings. Connecting with others facing similar struggles fosters understanding and reduces loneliness.
Family members are equally affected by ALS’s impact on mental health. Counseling can assist them in processing their emotions while learning how to best support their loved one.
Encouraging open conversations about fears and anxieties creates a safe space for expression. This dialogue is crucial for building resilience throughout the journey with ALS.
18. Emerging Research: Stem Cells, Gene Therapy, and Other Potential Breakthroughs
Emerging research in the field of Amyotrophic Lateral Sclerosis (ALS) holds promise for future therapies and better understanding of this complex disease. Scientists are exploring various innovative approaches, including stem cell therapy, which aims to repair or replace damaged motor neurons. This could potentially slow down the progression of ALS and improve patients’ quality of life.
Gene therapy is another area gaining traction. By targeting specific genetic mutations that contribute to familial forms of ALS, researchers hope to develop treatments that can alter disease pathways at their source. This approach may offer hope not only for those with inherited variants but also for sporadic cases through broader applications.
As technology advances, new methodologies such as CRISPR gene editing show potential in correcting harmful mutations directly within patient cells. Such breakthroughs could revolutionize how we think about treatment options for ALS.
Numerous clinical trials are underway testing these promising interventions. While results may take time to materialize, they reflect a growing commitment within the scientific community to tackle this devastating condition head-on.
The journey toward more effective solutions continues as researchers strive to uncover answers about ALS and its impact on breathing and muscle function. Each step forward brings new hope for individuals affected by this challenging disorder and highlights the importance of continued support for research initiatives aimed at finding a cure or improved management strategies for those facing trouble breathing due to ALS.


